What are the consequences of hydrosalpinx without treatment? Hydrosalpinx - what is it? Causes, symptoms, treatment and consequences of the disease. Hydrosalpinx of the fallopian tubes: treatment with folk remedies
A healthy woman is a happy woman. However, the female body is like a complex mechanism, where both minor difficulties and serious “breakdowns” are possible.
Clinical picture of hydrosalpinx
From a medical point of view, this is a very common disease of the female reproductive system and is the filling of the fallopian tubes with a cloudy yellowish liquid - transudate. The peculiarity of the disease is that periodically fluid can enter the vagina and be absorbed by its walls or flow into the uterine cavity, causing heavy clots of discharge.

Transudate affects the mucous membrane of the fallopian tubes, disrupting their natural function. Doctors tend to assume the toxic nature of the substance and, as a result, the risk of ectopic pregnancies, infertility, miscarriages increases and the chances of conception or successful procedure ECO. In addition, stagnation of fluid in the fallopian tubes causes the tubes themselves to become deformed, and the risk of infections occurs and develops.
Causes of the disease
Diseases of the reproductive system are characterized by a number of causes. Factors leading to the occurrence and development of hydrosalpinx may be:
- pathologies and structural anomalies of the pelvic organs;
- the presence and progressive formation of adhesions in the fallopian tubes and endometrial folds;
- impaired lymph circulation;
- difficult blood circulation in the pelvic organs;
- inflammation of the fallopian tubes;
- previously occurring inflammatory processes in the organs of the reproductive system;
- intestinal diseases;
- infections and sexually transmitted diseases, gonorrhea and chlamydia have a particularly strong impact on the female reproductive system.
Very often the disease is recognized by early stages is not possible due to the almost complete absence of symptoms. At later stages of the disease, the following may be observed:

Treatment of hydrosalpinx using alternative medicine methods
First of all, it is worth mentioning that treatment can be quite lengthy. However, having chosen recipes traditional medicine priority, you should definitely visit a doctor, remembering that in the case of an incorrectly selected set of measures, the sad result can be removal of the fallopian tubes and infertility.
Juice therapy
A body exhausted by illness needs help. Freshly squeezed juices are suitable as support.

Ancient recipes offer a wide range of variations herbal infusions and tinctures.

- Brew 5 grams of dried adonis herb and the same amount of crushed Adam's root in a glass of boiling water and leave covered for about two hours. The infusion, passed through a fine strainer, should be taken in small portions throughout the day.
- Freshly cut foxes from an aloe plant should be wrapped in foil and placed in the fruit drawer of the refrigerator for 72 hours. Grind the cooled leaves into a paste and mix it with melted bee honey in a volume six times greater than the amount of paste, and an equal volume of melted butter. Take two dessert spoons of honey-vegetable paste in a glass of warm milk in the morning and evening, for a course of eight weeks. The mixture must be stored under a saucer in the refrigerator.
- In parallel with the course of aloe pulp, it is recommended to drink a decoction of plantain seeds. To obtain it, pour two dessert spoons of seeds with half a liter of boiling water and place on the stove. Boil the mixture over medium heat for 7-9 minutes and cool. Take 1/3 cup three to four times a day for a course of eight weeks.
- Steam a dessert spoon of dry Adam's root herb with 200 ml of boiling water and leave. Strain the brewed infusion and drink in small sips throughout the day.
- Pour crushed dried ramishia flowers into a half-liter thermos and fill with boiling water to the top. Leave overnight and strain in the morning. Drink 2/3 cup of the decoction with each meal.
- Pour two tablespoons of dry adonis herb into 200 ml of boiling water and, covering with a saucer, wait until it cools. The entire strained infusion must be drunk within a day.
Teas with goldenseal or echinacea are also beneficial.
Pour four heaped tablespoons of washed oat seeds into a thermos and pour a liter of boiling water. Leave for at least 8-9 hours. After straining, the amount of infusion will be reduced by approximately half. It should be mixed with two tablespoons of honey and drunk 150 ml three times a day.
Decoctions of chamomile herbs, currant leaves, St. John's wort, sage, immortelle, mallow flowers, oak bark, and coltsfoot are also effective.
Make a mixture of dry herbs Adonis and Thamus in a 1:1 ratio. Pour 200 ml of boiling water over a dessert spoon of the collection and leave for several hours. The strained infusion should be drunk the day before.
Pour the washed red viburnum fruits with an equal volume of just boiled water and cook over high heat for 3-5 minutes, leave without removing the lid for 6-7 hours and pass through a sieve. The drink should be consumed without sugar, but a small amount of honey may be added.
Pour 10 grams of crushed dried ortilia herb into two glasses of boiling water and leave covered. You need to take the decoction 100-150 ml three times a day. It is advisable to drink the entire infusion completely.

It is useful to take 45-55 drops of alcohol tincture of galangal root, diluted in 100 ml of boiled water, on an empty stomach. The average course lasts 10-14 days.
In the same way, tinctures of cinquefoil and ortilia are taken.
Stir the alcohol infusion of boron uterus (one tablespoon) into 30 ml of boiled cold water. Take a dessert spoon of the diluted infusion with each meal for a month. This is followed by a ten-day break and the course is repeated.
Pour crushed white acacia flowers and crushed plant bark, totaling 15 grams, into a 200 ml jar and fill with vodka. Cover with a lid and leave in a dark place for 5-6 days. Acacia tincture is taken 25-30 drops half an hour before meals.
Aromatherapy sessions with oils of eucalyptus, cypress, sage, coniferous trees, and lavender provide a relaxing and strengthening effect.
Microclysters and lotions
Douching with herbal decoctions is widely used for diseases of the female genital organs. The temperature of the infusion should not be too hot; close to the temperature of the human body is considered optimal.

In addition, warm compresses are made with herbal decoctions on the lower abdomen and tampons soaked in infusions (not alcohol!) are inserted inside. These procedures will help relieve inflammation and reduce pain. It is important to carefully filter infusions from plant parts and keep all instruments properly clean. Ideally, the douching bag should be treated with an antiseptic solution before each use. Or pour boiling water over it.
- pharmaceutical camomile;
- sage;
- St. John's wort;
- calendula;
- mallow;
- Oak bark;
- coltsfoot;
- salvia;
- Potentilla (rhizome).
All of the herbs listed can be used alone or in collections. To prepare the infusion, you need to pour 25 g of herb into a liter of boiling water and leave, strain and cool to the desired temperature. The course of treatment varies from 20 to 30 days.
Standard appointment times medicinal bath- 30 minutes. The best temperature is 39-45 degrees. It is important to remember that for such a procedure the bath is filled to half.


It is important to remember that alternative medicine serves as a good support to basic treatment. Do not neglect the advice of a doctor, given the complexity and delicacy of the disease.
Video - Treatment of hydrosalpinx with folk remedies
Diseases of the female genital organs are dangerous not only because of their presence, but also because of their consequences. Particularly morally traumatic are those that lead to infertility. The great mission of becoming a mother loses its significance and oppresses the woman. Modern medicine seeks and finds ways to cure such ailments, restoring hope to women. Hydrosalpinx is one of these unpleasant diseases.
The disease is a pathological change that occurs in the fallopian tubes. Deviations in lymph and blood circulation lead to the accumulation of fluid (transudate) in the cavity of the fallopian tubes. Since the fallopian tube enters the uterus at one end and the other ends into the abdominal region, one of them is blocked, and then the fertilized egg is not able to reach the uterus and reach its mucous membrane. And inflammation is to blame. However, we will tell you more about the causes of the disease.
The prerequisites for the development of hydrosalpinx are salpingitis, adnexitis, salpingoophoritis - these are inflammatory processes that occur in the uterus, its appendages, and in the fallopian tubes themselves. They are characterized by the formation of scars and adhesions that affect all layers of the fallopian tube. As these adhesions grow, mucus accumulates in the cavity of the fallopian tube, leading to the formation of hydrosalpinx. Bacterial infections such as gonorrhea, syphilis, and chlamydia can also cause hydrosalpinx.
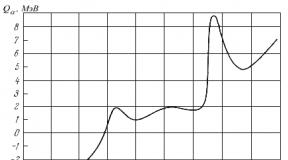
The mechanism of progression of hydrosalpinx looks like this: inflammation leads to the proliferation of connective tissue, adhesions and scars appear, they grow into the layers of the fallopian tube, disrupting the normal functioning of the muscular layer, fimbriae grow together, the patency of the lumen of the fallopian tube worsens, adhesions affect both ends of the tube and, as a result, , hydrosalpinx forms.
Having studied this mechanism, doctors determined the types of the disease.
Types and symptoms
The first division of hydrosalpinx into types is based on the number of cavities in the fallopian tube: 
- simple form - one cavity is formed
- follicular form - several cavities are formed
There are also forms of the disease that correlate with its course:
- acute
- chronic
Having decided on the forms, it would be logical to move on to their symptoms. Acute is characterized by:
- production of serous exudate
- temperature increase
- weakness
- cardiopalmus
- throbbing pain in the groin area
- pronounced blush on the cheeks, which is not typical on ordinary days
The chronic form develops slowly and over a long period of time, so there is no pain or other tangible signs, and the disease itself can only be detected with a pelvic ultrasound. If a lot of mucus has accumulated in the tubes, then the woman may feel a foreign body and heaviness in the groin area, and pelvic pain is possible.
There is another type of disease that is impossible to ignore - this is ventral hydrosalpinx. The adhesions in the fallopian tubes in this form have a loose structure and periodically break through, pouring out streams of mucus. A natural symptom of the disease is copious watery discharge.
Well, we’ve sorted out the forms, let’s move on to methods for diagnosing hydrosalpinx.
Diagnostics
Diagnosis of the disease is carried out in several stages. Let's list everything:
- Gynecological examination. When examining the uterus, the gynecologist palpates a tight, elastic formation located between the uterus and the ovary. It may have a round or ovoid shape. It is painless when pressed.
- Hysterosalpingography. This is an X-ray examination of the fallopian tubes, which determines the obstruction of the fallopian tubes. With ventral hydrosalpinx, the tube filled with a contrast agent resembles a “twisted sausage.”
- Ultrasound. An ultrasound shows the presence of a fluid formation between the ovary and uterus.
- Laparoscopy. Includes both research and treatment.
Once the diagnosis is established and confirmed, a treatment plan is drawn up.
Treatment
 Today, doctors offer two methods of treating hydrosalpinx - conservative and surgical. Both of them are aimed at resolving the fluid accumulated in the pipes and, ultimately, restoring their normal patency.
Today, doctors offer two methods of treating hydrosalpinx - conservative and surgical. Both of them are aimed at resolving the fluid accumulated in the pipes and, ultimately, restoring their normal patency.
Conservative method
The initial stage of the conservative method, as a rule, involves eliminating the inflammation that led to the appearance of hydrosalpinx. In addition, antibacterial and physical therapy are prescribed. In principle, such treatment has an effect only when the cause of hydrosalpinx is the previously mentioned diseases salpingitis, salpingoophoritis and adnexitis.
Thus, conservative treatment effectively affects the inflammatory process and is powerless in the fight against adhesions and scars. And methods such as microenemas from decoctions of sage, chamomile, St. John's wort, which traditional medicine advises, are only supportive methods of therapy and do not lead to a cure.
Operative method
The surgical method of treating hydrosalpinx, namely laparoscopy, is recognized as a radical and truly positive result. The surgeon performs plasty of the fallopian tubes, removing adhesions and expanding the lumen. In especially severe cases, when it is obvious that plastic surgery will not restore the functionality of the fallopian tubes, they are removed, since they represent a source of chronic infection.
Why is hydrosalpinx dangerous?
The disease disrupts the functioning of the fallopian tubes, destroys the mucous membrane, and slowly but surely leads to ectopic pregnancy or infertility. Without timely treatment, fluid accumulates between the adhesions, and a dangerous source of infection is constantly present in the woman’s body. This is a negative fact for the IVF procedure, which doctors resort to if infertility from hydrosalpinx cannot be avoided.
Be attentive and careful about your own health and do not exclude the joy of motherhood because of laziness or stupid delay in visiting the gynecologist.
Update: October 2018
One of the unpleasant consequences of inflammation of the appendages, in particular the fallopian tubes, is hydrosalpinx. According to statistics, this pathology occurs in 10–30% who are faced with the problem of pregnancy, since hydrosalpinx interferes with successful conception.
But with timely and adequate treatment, the onset of a long-awaited pregnancy is quite possible, so you should not try to get rid of this disease on your own, this only aggravates the pathological process and delays the wait for the joyful moment - the birth of a child.
Hydrosalpinx: what is it?
Hydrosalpinx is a disease of the fallopian tubes that results in disruption of their patency. The name of the pathology comes from Latin words, where “Hydro” is translated as liquid, and “salpinx” means pipe. The phrase often used by women - hydrosalpinx of the tubes - is incorrect, just like oilseed oil. A feature of the disease is the accumulation of fluid (transudate) in the lumen of the fallopian tube due to blockage of the internal and external openings of the oviduct, as a result of which it turns into a saccular formation.
There are:
- right-sided hydrosalpinx;
- hydrosalpinx on the left;
- bilateral hydrosalpinx.
It is incorrect to use such combinations as acute and chronic hydrosalpinx. This pathology is a complication of the inflammatory process of the fallopian tubes - salpingitis, which can be both acute and chronic.
An example of a diagnosis: Acute bilateral salpingoophoritis. Bilateral hydrosalpinx.
A little anatomy and physiology
The fallopian tube (synonyms: fallopian tube or oviduct) is a paired organ and is presented as a hollow tube with two lumens. The length of the oviduct reaches 10–12 cm, with the right tube being slightly longer than the left. One end of the oviduct opens into the uterine cavity, and the other ends with fimbriae (villi) and opens into the abdominal cavity, near the ovary. Through these openings, the abdominal cavity communicates with the woman's internal and external genitalia, which increases the risk of ascending infection, for example, with vaginitis.
The wall of the oviduct consists of three layers:
- external – represented by the peritoneum and protects the pipe from negative influences;
- muscular - formed by muscle fibers and thanks to which the tube makes peristaltic (contractile) movements towards the uterine cavity;
- internal, covered with ciliated epithelium, the cilia of which move in waves (flicker), which facilitates the movement of the fertilized egg towards the uterus; in addition, the glands located in the mucous layer of the tube produce a secretion that maintains the constancy of the internal environment of the oviduct and the viability of the egg, sperm and zygote.
The role of the fallopian tubes
The oviducts are essential for successful conception and implantation of a fertilized egg in the uterus. The functions of the fallopian tubes include:
- with the help of the fimbriae of the funnel of the tube, the matured egg released from the follicle is captured (the moment of ovulation);
- the egg moves to the ampullary section of the tube, where sperm are delivered from the uterine cavity;
- maintaining the viability of germ cells (sperm and eggs), preparing for their union, direct fertilization;
- maintaining the vital activity of a fertilized egg (zygote) in the tube until it moves into the uterine cavity;
- transportation of the zygote into the uterine cavity due to peristalsis of the oviducts and increased activity of the cilia of the ciliated epithelium.
The mechanism of pathology development
Impaired functioning of the fallopian tubes occurs due to inflammation, for example, against the background of salpingitis or salpingoophoritis. As a result, it begins to grow connective tissue and scars and adhesions form. The inflammatory process and adhesions affect all layers of the oviducts, with varying degrees of severity.
The villi of the ciliated epithelium die, and the muscle layer stops contracting (peristalsis disappears). Adhesions grow in the lumen of the fallopian tube, which impairs its patency, and the fimbriae of the funnel of the tube stick together. When the adhesions close both openings of the oviduct, mucus begins to accumulate in the resulting closed space, intensely, due to inflammation, produced by the glands of the epithelium of the inner layer of the tube. As a result, the tube expands, forming a hydrosalpinx or sactosalpinx. When the serous-mucosal contents of the tube suppurate, a pyosalpinx is formed.
In some situations (incomplete fusion of the fimbriae), a “ventilated hydrosalpinx” is formed, which periodically breaks through due to the pressure of the accumulated fluid. An increase in pressure occurs with a sudden change in body position, straining, or during hysterosalpingography. In this case, the transudate flows into the pelvis. Emptying of the oviduct with “ventilated hydrosalpinx” occurs systematically. The overflowing inflammatory fluid stimulates the formation of adhesions in the pelvis - a vicious circle is formed that maintains the existence of hydrosalpinx.
Causes of hydrosalpinx
The formation of hydrosalpinx is caused by the closure of the ampullary (middle) part of the fallopian medium, which is facilitated by a local infectious-inflammatory reaction. Infectious agents can penetrate into the cavity of the oviduct both ascendingly, from the underlying organs of the reproductive system (cervix, vagina, uterus), and descendingly through the bloodstream (bladder and kidneys, tonsils and intestines, appendix and others). Inflammation can be aseptic and occur in the presence of other gynecological diseases. The formation of hydrosalpinx occurs due to the following reasons:
- inflammation of the tubes, ovaries or appendages (salpingitis, oophoritis, adnexitis);
- inflammation of the uterus (endometritis);
- frequent and random change of sexual partners (sexually transmitted infections: chlamydia, myco- and ureaplasma, trichomonas, gonococci and others);
- tuberculosis of the female genital organs;
- wearing an intrauterine contraceptive;
- frequent hypothermia (weaken the immune system and activate opportunistic flora);
- abortions and diagnostic curettage of the uterine cavity;
- long-term vaginitis and vaginal dysbiosis;
- inflammation of the cervix and cervical canal;
- external endometriosis (causes aseptic inflammation and the formation of adhesions in the pelvis);
- adenomyosis;
- myomatous node in the area where the fallopian tube enters the uterine cavity;
- sexual infantilism (pipes are thin, long and crooked);
- damage to the oviducts during laparoscopy with the subsequent occurrence of aseptic inflammation.
The following factors predispose to the formation of a saccular formation in the pipe:
- neglect of the rules of intimate hygiene;
- stress, emotional stress;
- endocrine pathology: diabetes, diseases of the thyroid gland (weaken the body’s defenses).
But I would like to note that not always suffered and treated salpingitis or adnexitis ends in the formation of hydrosalpinx. With strong immunity and adequate and timely treatment, the inflammatory process in the tube disappears without consequences.
Symptoms
The clinical picture of the described pathology depends on the disease that caused it. With hydrosalpinx, which developed against the background of acute inflammation of the tubes, the symptoms are more pronounced. The patient is worried about febrile temperature, sharp, bursting pain in the groin (left or right), signs of intoxication: loss of appetite, lethargy and weakness. With the rapid accumulation of transudate in the ampullary section of the tube, the pain is bursting and pulsating.
In the case of chronic salpingitis, accompanied by the formation of hydrosalpinx, patients are often not bothered by anything. Often the only complaint is the inability to get pregnant, and hydrosalpinx is discovered during additional examination. But complaints of discomfort in the iliac regions, sensation of a foreign body in the groin, etc. are also possible. If there is ventral hydrosalpinx, then the woman may notice periodic heavy watery discharge from the genital tract (in the event of a rupture of the formation into the uterine cavity). When transudate spills into the pelvic cavity, adhesions increase in it, which is manifested by chronic pelvic pain syndrome. Sometimes the symptoms of saccular tube formation resemble acute surgical pathology (appendicitis, renal colic or intestinal colic).
Typical signs of chronic salpingitis and formed hydrosalpinx are:
- discomfort or minor It's a dull pain in the iliac region/regions;
- menstrual disorders;
- pathological discharge from the genital tract;
- absence of pregnancies.
Pregnancy due to hydrosalpinx
It is possible to become pregnant due to hydrosalpinx, but only if the tube is damaged on one side. Accordingly, the likelihood of conception is reduced by 50%. However, with this disease, the risk of tubal pregnancy and spontaneous abortion increases. Ectopic pregnancy is caused by damage to the ciliated epithelium in the affected tube and disruption of its peristalsis. As a result, the fertilized egg lingers in the oviduct for 4 or more days, where it implants and continues to develop.
Spontaneous termination of pregnancy due to saccular expansion of the tube is explained by several points:
- mechanical effect: periodically pouring fluid from the ventral hydrosalpinx washes the zygote from the surface of the endometrium, preventing it from implantation;
- the inflammatory transudate of the hydrosalpinx, entering the uterine mucosa, causes its damage and the development of endometritis, which makes implantation of the embryo impossible;
- there may be a toxic effect of the inflammatory fluid on the embryo, which leads to its damage and death;
- the sensitivity of endometrial receptors to female sex hormones decreases, which leads to disruption of the hormonal regulation of the uterine mucosa during the implantation process.
If hydrosalpinx is diagnosed on both sides, then pregnancy cannot occur naturally. In such cases, they resort to assisted reproductive technologies (IVF), although the effectiveness of in vitro fertilization and subsequent gestation is reduced several times (2 – 5).
If pregnancy nevertheless occurs against the background of an existing saccular expansion of the tube, then it can terminate spontaneously in the early and late stages. Therefore, all pregnant women with hydrosalpinx are at high risk for miscarriage. Treatment of the disease is postponed until the postpartum period.
Diagnostics
Diagnosis of this complication begins with a gynecological examination. When performing bimanual palpation, hydrosalpinx can be felt as a tight-elastic and elongated formation on the right/left or on both sides. There may be minor pain on palpation of the appendage area or no pain at all. But with a slight expansion of the oviduct, the doctor may not palpate the formation and prescribe additional research methods:
Ultrasound transvaginal sensor
The presence of a saccular formation on one or both sides, located between the uterus and the ovary, its size and shape are determined. It is possible to visualize the septa in the formation (follicular hydrosalpinx). The formation is filled with hypoechoic fluid and has its own thick capsule.
Hysterosalpingography
This method consists of introducing a contrast agent (under pressure) into the uterine cavity through the cervical canal. Then x-rays are taken. Hysterosalpingography allows you to determine the patency of the tubes - contrast is visualized in the pelvis and identify hydrosalpinx. If there is a complication, the fallopian tube looks tortuous and thickened, and accumulated contrast is found in the enlarged ampullary section.
Laparoscopy
It is carried out for diagnostic and therapeutic purposes. During laparoscopic surgery, thickened fallopian tubes are revealed, the fimbriae at their ends are swollen and hyperemic, and the wall of the tube is thinned and translucent, its cavity is filled with watery contents.
In addition to instrumental examination methods, it is necessary to be tested for sexually transmitted infections (chlamydia, myco- and ureaplasma, cytomegalovirus, HPV and herpes virus).
Treatment
If hydrosalpinx is detected, a woman is strongly recommended to undergo treatment, because the longer this pathology exists, the more intensively adhesions form in the pelvis, which reduces the chances of conception and increases the risk of miscarriage or ectopic pregnancy. Unfortunately, many patients think of this disease as not serious (it doesn’t hurt, so it’s not dangerous) and delay their visit to the gynecologist. Sometimes this leads to irreversible consequences: the absolute impossibility of conceiving naturally and the need to resort to IVF.
But how to treat this pathology? Treatment for hydrosalpinx is carried out in two stages. The first stage of treatment is conservative therapy. If there is an acute inflammatory process of the appendages or an exacerbation of a chronic one. First of all, antibiotic treatment is prescribed. The duration of the course and dosage of antibacterial drugs are selected individually, taking into account the identified pathogens and their sensitivity to drugs.
The main line of conservative therapy is stimulation of the immune system. For this purpose, immunomodulatory drugs are prescribed:
- immunofan;
- lycopid;
- imudon;
- Thymalin;
- taktivin;
- aloe injections;
- immunal;
- autohemotherapy (intramuscular injection of a woman’s own venous blood).
Also, to stimulate the immune system, taking and parenteral administration of vitamins is indicated. Physiotherapeutic procedures are widely used, although it is impossible to achieve complete cure of hydrosalpinx and resorption of adhesions with their help:
- magnetophoresis;
- electrolytes (calcium, magnesium);
- electrical stimulation of the fallopian tubes;
- endovaginal vibration massage.
Hirudotherapists are confident that it is possible to get rid of this disease by resorting to the method of treatment with leeches. Such a statement has no basis in scientific evidence or confirmed statistical data.
Traditional methods
Most patients believe that hydrosalpinx can be treated folk remedies. Doctors allow the use traditional methods, but only as an addition to the first (conservative) stage of therapy. Traditional medicine will not help get rid of the disease, but will only eliminate a number of symptoms: reduce pain, somewhat slow down the progression of inflammation and adhesions, and more or less normalize the menstrual cycle. Among the recommended folk remedies, it is permissible to use:
- taking pumpkin, potato and nettle juice (separately or in a mixture);
- microenemas with medicinal herbs(pharmacy chamomile, calendula, oak bark);
- taking a mixture of aloe leaves, butter and honey;
- taking oat infusion;
- taking juniper baths (an infusion of berries and juniper branches is poured into the water; the water in the bath should be warm, but not hot);
- infusion of adonis;
- infusion of a mixture of herbs (chamomile, currant leaf, sage, St. John's wort).
Once again I would like to remind you that it is impossible to achieve a complete cure of the disease using traditional medicine methods.
Surgery
The second stage of treatment for this complication is surgical intervention. If hydrosalpinx is present, treatment without surgery does not make sense. As long as the focus of inflammation remains in the pelvis, adhesions will continue to form, pain will persist and the chances of fertilization will decrease.
Today, laparoscopy is used as a surgical intervention for hydrosalpinx. Laparoscopic treatment of saccular formation in the tube is the most gentle and effective surgical intervention. During laparoscopy, depending on the condition of the tubes, the age of the patient and her desire to become pregnant, the following types of surgical intervention in the anatomy of the oviduct are performed:
- salpingo-ovariolysis - adhesions around the oviduct and ovary are dissected, their anatomical location is restored, and adhesions in the lumen of the fallopian tube are also separated;
- fimbryolysis and fimbryoplasty – the fimbriae of the final section of the tube, which are adjacent to the ovary, are freed from adhesions, the inflammatory transudate is removed from the tube, and, if necessary, fimbriae plastic surgery is performed;
- salpingostomy and salpingoneostomy - they form a new hole in the ampullary section of the oviduct or are freed from adhesions of the anatomical hole (minus salpingoneostomy - the new hole closes very quickly);
- tubectomy – removal of a tube/tubes (performed in women over 35 years of age or if it is impossible to restore the patency of the oviduct and eliminate hydrosalpinx).
But even in the case of a successful operation, preserving the tube and restoring its patency, the oviduct does not function as before. The villi of the ciliated epithelium either lose their mobility, or the epithelium itself atrophies, and the muscle layer is not able to contract as before, that is, the peristalsis of the tube is disrupted, so patients are included in the risk group for ectopic pregnancy, and pregnancy is recommended through IVF.
Question answer
How dangerous is this disease?
The presence of hydrosalpinx increases the likelihood of an ectopic pregnancy several times. In addition, hydrosalpinx almost always leads to infertility. A saccular formation in the pipes that increases in volume may burst or fester (pyovar).
Are there any restrictions necessary for this disease?
Yes, definitely. Firstly, physical activity should be avoided (vibration, straining, sudden changes in body position: somersaults, bending, jumping). Secondly, avoid excessive activity during sexual intercourse, which increases pain. In addition, it is not recommended to sunbathe and visit a solarium, as well as visiting baths, saunas and taking hot baths, which can provoke an exacerbation of the inflammatory process. It is undesirable to swim in the pool and open reservoirs, as local hypothermia will also provoke an exacerbation. It is prohibited to drink alcohol, including low-alcohol drinks, which suppresses the immune system.
What is the prognosis for pregnancy after laparoscopic surgery for this disease?
With the patency of the tube restored and the hydrosalpinx removed, conception naturally and pregnancy occurs in 60–75%, and the probability of an ectopic pregnancy does not exceed 5%. If the tube is removed, the effectiveness of IVF is 30 - 35%.
For 3 to 4 weeks it is necessary to refrain from physical activity and observe sexual rest. You should also follow a diet that limits the consumption of spicy, pickled and salty foods, fried and fatty foods, fast food and canned food.
Hydrosalpinx (from Greek) is a pathological condition characterized by excessive accumulation of exudate (liquid seeping from small blood vessels during inflammation) in the cavity of the fallopian tube.
Hydrosalpinx occurs when fluid outflow is impossible due to blockage of the tube lumen and can be localized on both the left and right, or on both sides. If blood and lymph circulation is impaired, the fallopian tube becomes impassable in a certain area, adhesions form in it due to acute salpingitis (inflammation of the tube).
Isolated damage to just the fallopian tubes is quite rare. As a rule, the ovaries and uterus also become inflamed.
Salpingitis- this is an inflammation of the uterine (fallopian) tubes as a result of infection from the uterine cavity and other pelvic organs. Follicular salpingitis can be caused by sexually transmitted infections, usually gonorrhea and chlamydia.
There are simple hydrosalpinx when one closed cavity appears in the pipe as a result of the adhesion process, and follicular hydrosalpinx, if the lumen of the pipe is divided into several cavities.
After the formation of cavities in the presence of an inflammatory process, exudate (liquid) begins to accumulate in the fallopian tubes. The pipe wall stretches (up to several cm in diameter) and becomes so thin that liquid can be seen through it. At times, the fluid in the fallopian tubes is absorbed by the wall of the tube, and the hydrosalpinx decreases. But after some time, due to the presence of adhesions, it occurs again. Therefore, the disease is characterized by a chronic relapsing (repeating) course. As a rule, the pathological process occurs on both fallopian tubes.
Sactosalpinx is the same as hydrosalpinx , but exudate (serous, bloody or purulent fluid seeping into the fallopian tube from small blood vessels) can pour out through the uterus from the cavity formed as a result of adhesions in the fallopian tube. The disease occurs as a result of the inflammatory process and the formation of adhesions in the ampullary part of the fallopian tube and, as a rule, only on one side.
Pyosalpinx Thisaccumulation of pus in the fallopian tube as a result of overgrowth of the ampullary and uterine part of the tube with purulent salpingitis. Over time, the walls of the pyosalpinx thicken and the mucous membrane is destroyed. The pyosalpinx is almost always surrounded by extensive fusions with neighboring organs - the ovary, omentum, posterior wall of the uterus, and intestinal loops. The pus in the pyosalpinx is initially liquid, but becomes thick over time.
Pus from the pyosalpinx can break into the rectum (good prognosis), less often - into the bladder, into the vagina (with the formation of a tubovaginal fistula) and into the abdominal cavity. In this case, infection may cause diffuse peritonitis, requiring urgent laparotomy.
Symptoms of hydrosalpinx (sactosalpinx)
One of the symptoms of hydrosalpinx is an increase in body temperature. In acute salping if the secretion (exudate) released in the tube is serous, then the disease occurs with a subfebrile body temperature of 37.5ºC, serous-purulent - 38ºC, purulent - up to 39ºC.
The inflammatory process is accompanied by weakness, throbbing pain in the groin area. Tachycardia (rapid heartbeat) may occur.
For chronic (long-term and sluggish) salpingitis gluing of fimbriae (fimbriae of the fallopian tube) can occur painlessly. In this case, the inflammatory exudate gradually accumulates in the pipe. A small accumulation of fluid in the fallopian tube during an inactive process, as a rule, does not cause pain and can be detected accidentally during a pelvic ultrasound.
A symptom of hydrosalpinx (sactosalpinx) may be cramping pain in the pelvic area. , accompanied by copious leakage of fluid from the vagina (with a breakthrough and outflow of exudate). The liquid can be transparent or may have a yellowish tint.
More often, a woman may notice periodic or constant watery discharge from the genital tract - when the sactosalpinx empties into the uterus and vagina. When a tube ruptures, a sharp pain occurs in the abdomen; when fluid suppurates (pyosalpinx), weakness, intoxication, and increased body temperature occur (pain may be absent, because sensitivity is reduced in the highly stretched walls of the fallopian tube). A woman’s inability to conceive is also noted.
Hydrosalpinx can form in the fallopian tubes on the left, right, and also on both sides. With a significant increase in the fallopian tube, a constant feeling of heaviness appears, a sensation of a foreign formation in the corresponding groin area (left or right). For chronic sluggish salpingitis body temperature and basal temperature, as a rule, are not elevated.
Diagnosis of the disease
Hydrosalpinx (sactosalpinx) usually diagnosed using hysterosalpingography (HSG). This is an x-ray procedure in which a radiopaque fluid is injected into the uterine cavity and the shape of the uterus and the patency of the fallopian tubes are assessed. If the pipes are not passable, then liquid accumulates in the pipe. When the fallopian tubes are patent, fluid from the terminal section of the tubes pours into the abdominal cavity.
During an ultrasound of the pelvic organs, the presence of a smooth-walled unilateral or bilateral tumor-like formation in the area of the uterine appendages is diagnosed. To confirm the diagnosis, diagnostic laparoscopy is performed. A small puncture (5-10 mm) is made in the abdominal area and a thin optical instrument - a laparoscope - is inserted into the abdominal cavity, with which the fallopian tubes, ovaries and uterus are examined.
If hydrosalpinx (sactosalpinx) is detected, microsurgical instruments are introduced through additional incisions, with the help of which the necessary operations are performed to remove pathologically altered sections of the tubes, reconstruct the fallopian tubes, dissect adhesions, etc.
Treatment of hydrosalpinx (sactosalpinx)
Timely detection and treatment hydrosalpinx(actually salpinx) is due to the risk of atrophy of the ciliated epithelium of the fallopian tubes . The rhythmic movements of the cilia that line the fallopian tube help propel the egg through the fallopian tubes into the uterine cavity. With atrophy of the cilia, the risk of ectopic (tubal) pregnancy and infertility increases significantly.
In addition, this pathology is a source of constant infection, where, like in an incubator, ideal conditions are created for the proliferation of bacteria. With the long-term existence of the pathological process and the absence of adequate treatment, adhesions are formed that limit the source of inflammation. Thus, an adhesive process is formed in the pelvis, causing chronic pain (plastic peritonitis), which increases the risk of ectopic pregnancy and infertility.
In case of acute salpingitis and the formation of hydrosalpinx (sactosalpinx, pyosalpinx), hospitalization is necessary. Antibiotics, antihistamines, and cold applied to the pelvic area are prescribed.
Treatment methods for hydrosalpinx
Treatment of hydrosalpinx (sactosalpinx) with conservative methods is almost impossible. Surgical laparoscopy using endovideosurgical instruments is indicated, which makes it possible to most effectively restore the patency of the fallopian tube. Reconstructive plastic surgery of the fallopian tubes is performed. In case of rupture or suppuration (pyosalpinx), the fallopian tube can be partially or completely removed, because exudate is a breeding ground for bacterial growth. Control hysterosalpingography is performed.
Immediately after the operation, a course of physical therapy is carried out to prevent the development of adhesions. Physiotherapeutic procedures (magnetophoresis, laser phoresis, electromagnetophoresis) allow you to administer the drug directly to the site of inflammation. Mud therapy, ultrasound, and diathermy are also used.
Removal of tubes before IVF pregnancy
Women planning pregnancy with long-standing hydrosalpinx (sactosalpinx), after preliminary physiotherapeutic preparation, laparoscopy is performed to restore the patency of the fallopian tubes. Unfortunately, when the tubes are restored, their function may be damaged.
In a tube with hydrosalpinx, the folding of the tube mucosa, necessary for normal function, is disrupted. The ciliated cilia inside the tube that propel the egg do not recover, and scars may form on the tube. In addition, the number of receptors for the main hormones estradiol and progesterone sharply decreases. These factors can often lead to ectopic pregnancy.
If this pathology is present in one fallopian tube and the other tube is patent, pregnancy is theoretically possible. However, the presence of a focus of chronic infection in the pelvis significantly reduces the chance of pregnancy, because the inflammatory process is toxic to the embryo.
If the fallopian tube is removed and the other fallopian tube is patent and there is regular ovulation, the chance of getting pregnant on your own is about 50%.
Removal of one or both fallopian tubes using laparoscopy does not reduce a woman’s sexual desire, does not cause disruption of menstrual function, hormonal levels and does not entail negative consequences on other body functions.
At bilateral hydrosalpinx Conceiving naturally is not possible. Removal of tubes before IVF is indicated. If you have hydrosalpinx on the left or right, it is recommended to first remove it and only then try to get pregnant.
Hydrosalpinx and IVF
Scientists have proven that the fluid that accumulates in the cavity of the altered fallopian tube is toxic to the embryo, because it contains microorganisms, dead cells of the fallopian tube mucosa, lymphocytes and other toxic agents. Flowing from the cavity of the tube into the uterine cavity, this fluid inhibits the further development of the embryo. Exudate flowing from the fallopian tube contains prostaglandins and cytokines that disrupt the normal functioning of the endometrium and its ability to implant an embryo.
With severe disease, a woman’s ovaries respond more poorly to stimulation of superovulation in an IVF cycle.
Removal of fallopian tubes with hydrosalpinxes before the IVF procedure leads to a sharp increase in the frequency of pregnancy - from 10% on average with hydrosalpinx to 30 - 35% after removal of diseased tubes. Moreover, the prognosis significantly improves precisely in the case of removal of the tubes, and not in attempts to restore the patency (tubostomy, fimbrioplasty) of the affected tubes. Therefore, IVF for hydrosalpinx is indicated only after removal of the fallopian tubes.
Previously, concerns were expressed that removal of the tubes, even if altered, could lead to disruption of the blood supply and nervous regulation of the ovaries. Studies conducted on the removal of the affected tubes before the procedure did not reveal any difference in the condition of the ovaries, as well as in the response of the ovaries to stimulation, the quality of the eggs obtained, the fertilization rate and the quality of the embryos obtained between groups of women in one of which hydrosalpinxes were removed, and in the other the tubes were initially removed were normal.
Conducted studies indicate the need to remove fallopian tubes with hydrosalpinx (sactosalpinx) before the IVF procedure.
Hydrosalpinx is one of the diseases of the fallopian tubes. According to statistics, about 10-30 percent of female representatives suffer from this pathology. In particular, this greatly affects when planning a pregnancy, which the disease creates an obstacle to.
Hydrosalpinx is a disease in which the obstruction of the tubes occurs.
The peculiarity of this pathology is the accumulation of fluid in the pipes as a result of blockage of the internal and external oviduct. Against this background, something like a bag is formed.
The penetration of infectious pathogens occurs through the bloodstream, which comes from the kidneys, Bladder, intestines. The inflammatory process can also be provoked by gynecological pathologies.
The main reasons why hydrosalpinx may develop are:
Among the predisposing factors that significantly increase the risk of pathology formation are:
- frequent stressful situations;
- emotional stress;
- diabetes;
- thyroid diseases;
- failure to comply with personal hygiene rules.
It should also be noted that not in all cases, salpingitis or andexitis can result in the development of hydrosalpinx.
With healthy immune system, as well as timely treatment, inflammatory processes in the fallopian tubes are eliminated and do not cause any unpleasant consequences.
Classification and symptoms
There are three types of disease:
- right-sided hydrosalpinx;
- left-handed;
- double-sided
In addition, depending on the course of the disease, inflammatory processes can be acute or chronic.
The clinical manifestations of the disease will largely depend on the underlying cause that contributed to its development. If the provocateur of hydrosalpinx is inflammatory processes of the fallopian tissues, then the symptoms will be more pronounced.
The patient exhibits signs of body intoxication:

When transudate accumulates in the middle section of the tube, the pain will be pulsating.
If hydrosalpinx occurs against the background of chronic salpingitis, symptoms may not manifest themselves. The only thing that can worry the patient is the inability to get pregnant. In this case, the presence of pathology will be detected only during the examination of the causes of infertility. Pain during sexual intercourse and the feeling that there is a foreign body in the groin may be bothersome.
If the disease has a ventilatory form, a woman may periodically experience watery vaginal discharge.
Characteristic signs of chronic salpingitis with the manifestation of hydrosalpinx are:
- menstrual irregularities;
- inability to get pregnant;
- discharge from the genital tract;
- minor pain in the iliac region
In the case when liquid is poured into the pelvis, the risk of adhesions increases significantly. This is accompanied by a syndrome of chronic pain in the pelvis.
Doctors tell us why women have pain in the groin area, watch the video:
Diagnostics
When the first signs appear that indicate a suspicion of the development of hydrosalpinx, you should immediately seek medical help. After examining and studying the medical history, the gynecologist will be able to make a preliminary diagnosis.
For the final diagnosis of pathology, additional examinations can be used:
- Carrying out an examination on a gynecological chair. The vagina is examined with both hands, the size of the ovaries and uterus is determined, and pain in the fallopian tubes is detected;
- Ultrasound (ultrasound examination). Using this method, it is possible to determine the formation of fluid in the pelvis;
- Hysterosalpingography. Determines the patency of the fallopian tubes by introducing a contrast agent;
- Polymerase chain reaction. Identifies sexually transmitted pathologies;
- Laparoscopy. Carrying out this operation is not only a method for diagnosing hydrosalpinx, but is also carried out for preventive and therapeutic purposes.

Treatment of hydrosalpinx
After a diagnosis confirming the presence of this disease is made, a woman must undergo the course of medical therapy prescribed to her.
It is very important that measures to eliminate the pathology are taken in a timely manner, otherwise there is a high probability of an advanced process of formation of adhesions in the pelvis, which in most cases leads to ectopic pregnancy, miscarriages or infertility.
Treatment measures include two stages:
- conservative methods;
- surgical intervention.
Drug therapy
In case of inflammatory processes in the appendages or exacerbation of the disease, a course of antibiotics is necessarily prescribed.
The duration and dosage are determined only by the attending physician in each case individually. Factors such as sensitivity to medicines and type of pathogen.
The main goal of conservative treatment is to restore and maintain the immune system.
For this purpose, immunomodulatory drugs are prescribed:

Despite the fact that it will not be possible to completely cure the disease with their help, their beneficial effects together with taking medications have been noted for a long time.
Physiotherapeutic methods include:
- electrophoresis;
- vaginal vibration massage;
- Magnetic cutter
Surgery
If surgical intervention is not used in the treatment of hydrosalpinx, there will be no effect.
 Until the source of the inflammatory process is directly suppressed, the formation of adhesions in the pelvis will continue. This contributes to the persistence of pain and increases the risk of infertility.
Until the source of the inflammatory process is directly suppressed, the formation of adhesions in the pelvis will continue. This contributes to the persistence of pain and increases the risk of infertility.
Today, a method such as laparoscopy is widely used. This is a more gentle way. During the operation, various types of surgical intervention can be used.
The choice depends on the general condition of the patient, the degree of pathology and the desire to become pregnant:
- Fimbryoplasty. The main goal is to free the fimbriae of the terminal section of the oviduct from the formed adhesions. If necessary, their plastic surgery can be performed;
- Tubectomy. Tubal resection is performed;
- Salpingostomy– an additional hole is formed in the middle section of the oviduct;
- Salpingo-ovariolysis– dissection of adhesions located along the perimeter of the ovaries, restoration of their position.
It should be noted that even if the operation is successful, the oviduct still loses its ability to function normally. In view of this, this category of patients is at risk for ectopic pregnancy.
Traditional methods of treatment
Before using any traditional medicine for treatment, you must first discuss this with a specialist. If the complex is incorrectly selected, there is a high probability of developing adverse consequences, which can lead to removal of the uterine tubes and infertility.
Herbal infusions and oils

Juice therapy
To maintain a depleted body, it is not a bad idea to drink freshly squeezed juices made from young nettles, potatoes or pumpkins. You can also add carrot juice to them.
Phytotherapy

Baths
As a rule, a medicinal bath should last thirty minutes. Water temperature is within 39-45 degrees. To carry out such procedures, it is necessary to fill the container only to half.
- In a separate container, dilute 8 tablespoons of clay with a liter of water. As the mixture begins to swell, stir it to prevent lumps from forming. After the liquid has cooled, lower your hands into it for 15 minutes, then only your feet for the same time. The procedure should be repeated up to 4 times a day. The break is for three days.
- The clay mixture is prepared according to the scheme described above and poured into a bathtub filled with water. The whole body is completely immersed. After taking it, you need to wear warm clothes and drink any of the herbal infusions, for example, chamomile tea.
Read also...
- Will I get married? Fortune telling online. Fortune telling for a new acquaintance. Fortune telling with playing cards Fortune telling by a friend
- Morozov Nikolay Aleksandrovich Nikolay Morozov Narodnaya Volya
- You can cook French fries in the microwave How to make your own French fries in the microwave
- Crispy pickled cucumbers in jars