Coxarthrosis (arthrosis of the hip joint). Causes, symptoms, diagnosis and treatment of arthrosis. Types of arthrosis Types of arthrosis and their diagnosis
To eliminate the symptoms of cervical osteochondrosis, the following groups of drugs are used:
- Pain syndrome - analgesics and anti-inflammatory drugs (ketorol, oxadol), muscle relaxants (milgamma, baclofen);
- Pain in the head - vasodilators (no-spa, papaverine) and nootropics (phenibut);
- Dizziness - drugs that improve microcirculation in brain tissue (trental, cinnarizine);
- Paresthesia (change in sensitivity) - B vitamins (milgamma, neuromultivitis).
Painkillers
The pain that occurs with cervical osteochondrosis is caused by several factors:
- Inflammation in the area of the damaged disc - destroyed disc tissue releases substances that trigger an inflammatory reaction. Blood flow to the affected area increases, swelling and compression of pain receptors occurs.
- Compression of the spinal nerve root - tissue swelling that occurs due to inflammation compresses the nerve trunk, causing a person to feel pain.
- Muscle spasm - a damaged nerve root sends a pathological signal to the neck muscles, causing them to contract. Prolonged tension leads to the accumulation of lactic acid in them, to which muscle receptors react - they send pain impulses to the brain.
To effectively eliminate pain, you must address all the causes of its occurrence. The following drugs are used for this:
- Celecoxib disrupts the production of inflammatory substances, due to which it has a pronounced anti-inflammatory effect. Eliminates swelling and pain.
- Baclofen - relaxes spasmodic muscles. The drug acts on inhibitory receptors in the brain and in nerve synapses - places where information is transmitted from one nerve cell to another. Thus, the transmission of pain impulses from the muscles and pathological impulses from the pinched nerve root are inhibited. The muscles relax, the pain disappears.
- Oxadol - affects the perception of pain in the brain. Activates endorphin receptors in the brain, thereby reducing pain sensitivity.
Dizziness with osteochondrosis occurs as a consequence of insufficient blood supply to the brain.
In close proximity to the cervical vertebrae there passes a paired vertebral artery, which carries blood to the brain.
Inflammatory swelling in the spine or a herniated disc compresses the artery, narrowing its lumen.
Blood flow to the brain deteriorates, a person feels dizzy, spots flash before the eyes, and tinnitus occurs.
Numbness in the hands occurs when the nerve root, which is responsible for sensitivity and movement in the upper extremities, is compressed. The nerve impulse from it gets distorted into the brain, so the person feels crawling, tingling and numbness.
Changes in nervous regulation gradually lead to deterioration of blood circulation in the upper extremities. This increases the discomfort, in addition to which muscle weakness and chilliness of the hands appear.
To cope with pathological changes, you should take:
- Mydocalm tablets– contains B vitamins (1 and 6). They are necessary for the restoration of the nerve fiber and the transmission of impulses along it. They stimulate the production of a protective fatty film that covers the nerve from the outside. Thanks to this, nerve sensitivity is restored and hand numbness is reduced.
- Neuromultivit is a multivitamin preparation that also contains B vitamins.
- Trental (pentoxifylline) – has a vasodilating effect and improves blood flow. Trental increases blood flow to the brain and improves microcirculation in its tissues. Dilates blood vessels in the upper extremities, eliminates the feeling of chilliness and numbness in the hands.
- Cinnarizine – improves blood microcirculation in brain tissue. The drug dilates blood vessels and reduces blood viscosity. Eliminates tinnitus, dizziness, and flickering of eyesight.
For headaches
Headache with cervical osteochondrosis has several causes:
- deterioration of blood supply to the brain;
- irritation of the spinal nerve (develops “cervical migraine”);
- disruption of the outflow of cerebrospinal fluid from the cranial cavity;
- reflection of pain from the cervical spine;
- compression of the sensitive nerve endings that innervate the occipital and temporal parts of the head.
A combination of an anesthetic drug with a vasodilator will effectively eliminate headaches. You can take analgin together with papaverine or no-shpa.
Vinpocetine is a drug for improving cerebral circulation. It dilates blood vessels, improves the absorption of glucose and oxygen by nerve cells. Vinpocetine reduces blood viscosity, thereby improving microcirculation. Protects nervous tissue from the harmful effects of hypoxia (lack of oxygen).
If the pain is of an excruciating bursting nature, accompanied by vomiting, then most likely it is caused by a violation of the outflow of cerebrospinal fluid from the cranial cavity. To alleviate the condition, the doctor may prescribe a diuretic drug - diacarb.
Diacarb reduces the production of cerebrospinal fluid and at the same time enhances the removal of fluid from the body. Quickly relieves headaches, but you can take it for no more than 5 days.
Cervicothoracic osteochondrosis is characterized by pain along the ribs, in the abdomen, and in the region of the heart. They are combined with headache, dizziness, neck and back pain. Severe pain syndrome requires the prescription of potent analgesics:
- ketorol;
- tramadol;
- Nurofen.
If there is severe destruction of the intervertebral discs and an inflammatory reaction, the doctor may prescribe glucocorticoids, for example, prednisolone tablets. The drug has a powerful anti-inflammatory effect due to disruption of the synthesis of certain biologically active substances.
The listed drugs must be combined with tablets for the treatment of cervical osteochondrosis.
Osteochondrosis is a chronic disease, so it occurs with periods of exacerbation and remission.
During an exacerbation, a person experiences severe pain, to eliminate which the doctor prescribes analgesics, muscle relaxants, and anti-inflammatory drugs.
Most of them should not be taken for a long time as they cause side effects.
During remission (absence or minimal manifestations of the disease), it is recommended to take tablets that improve blood supply to the brain, B vitamins, nootropics (drugs to improve brain activity), and chondroprotectors.
Damage to the cervical spine often has a pronounced negative impact on a person’s psyche and mood. There are several reasons for this: malnutrition of the brain, changes in the circulation of cerebrospinal fluid, and constant headache.

Mild herbal preparations can be prescribed: valerian tablets, novopassit, afobazole. In severe cases, they resort to the anticonvulsant drug carbamazepine. It reduces the excitability of the cerebral cortex and affects the exchange of neurotransmitters (substances that are responsible for transmitting information between cells). Thanks to this, carbamazepine eliminates irritability, anxiety, and depression.
Brain hypoxia can lead to disorders of thinking and memory. A person notices that it is more difficult for him to concentrate on work, fatigue sets in faster, and habitual mental operations are not possible. Drugs from the group of nootropics can cope with these phenomena.
Nootropics protect cortical neurons from the harmful effects of hypoxia and normalize their metabolism. They improve mental functions, memory, reduce anxiety and depression. Representatives of this group are glycine, phenibut, and avifen.
In any case, the selection of a treatment regimen should be carried out by a specialist - only he is able to take into account all parts of the pathological process and prescribe the most suitable drugs.
The cervical spine consists of seven segments, between which discs are located. The neck is the most vulnerable and mobile part of the spine, which bears most of the load: turning the head, bending, static postures.
The muscles supporting this section are the weakest, and this is precisely the first reason for the appearance of osteochondrosis. It is also worth noting the fact that most people are engaged in sedentary work, which negatively affects the spine.
Doctors diagnose four stages of osteochondrosis, each of which indicates the degree of damage to the discs.

| Therapy | Description |
|---|---|
| Magnetotherapy | The magnet helps improve blood circulation, reduce swelling, and reduce pain. Procedures with a magnet can be carried out at home by applying the device to the areas where pain is localized. Treatment with a magnet is prohibited at elevated temperatures, arterial hypotension, blood diseases, acute inflammatory processes |
| Darsonval | Darsonval is a device that affects human skin with alternating current, which arises from a tube filled with gas. When current is applied to problem areas of the neck, blood circulation improves, the transmission of nerve impulses is regulated, and the pain threshold is reduced. After the procedures, a person feels a surge of strength, his mood improves, and the feeling of fatigue disappears. Darsonval also helps to increase metabolic processes |
| Electrophoresis | This is one of the most effective methods of delivering medicine deep into the layers of the skin without pain or discomfort. Electrophoresis uses low currents, which are supplied to special plates. Tampons with medications - painkillers or anti-inflammatory drugs - are placed under the plates. Due to the low electrical conductivity of the dermis, the medicine, under the influence of electric current, penetrates deep into the skin, directly to the site of pain. |
| Ultrasound for cervical osteochondrosis | Ultrasonic waves penetrate deep into the skin and muscles, heating them by 2-3 degrees. Thanks to vibration and heating, blood circulation improves in the painful area, muscles relax, which helps relieve pain. To make the procedure as effective as possible, it is recommended to apply an anti-inflammatory or analgesic ointment to the skin before using ultrasound. Under the influence of waves, the medicine will have its therapeutic effect much faster. Using this method, you can achieve stable remission in 10-12 procedures |
Kinesiology
Anti-inflammatory drugs
With osteochondrosis of the thoracic region, a person suffers from pain in the back, in the area of the heart, stomach, and along the ribs. It is often painful for a person to take a deep breath or lie on one side. To help cope with the symptoms of the disease:
- diclofenac, dolobid, meloxicam;
- sirdalud, melliktin;
- ketorol, analgin;
- pentoxifylline;
- traumeel
With osteochondrosis of the lumbar region, the patient is bothered by pain in the lower back with radiation to the perineum and thigh, lumbago, difficulty urinating and defecating.
The following tablets will help:
- diclofenac, lornoxicam, meloxicam;
- mydocalm, sirdalud;
- milgamma and B vitamins;
- ketorol;
- pentoxifylline, aminophylline.
Effective remedies for annoying osteochondrosis can be prepared at home:
- The infusion of the string should be prepared according to the following recipe: take a spoonful of herbs and add boiling water. Wait 4 hours, strain and take 0.5 cups.
- A decoction of string is easy to prepare. To do this, you need to purchase this herb at the pharmacy and pour boiling water over a tablespoon of dry leaves - 2 cups. Set on low heat, cook for 3 minutes. Strain the broth and take 1/3 cup 3 times throughout the day.
Among the means for external treatment of the disease, there are also the most effective:
- Adam's root tincture involves using the root itself - 200 g, vodka - 0.5 l. Grate the product, add vodka, and place in a dark place for 5 days. The finished product is used to rub the affected cervical, thoracic or lumbar spine. This treatment provides deep heating, affecting the nerve endings.
- An ointment for rubbing the cervical, thoracic or lumbar region should contain the following herbs: knotweed root, St. John's wort, mint, pine buds, celandine, eucalyptus leaf. All ingredients are taken in equal proportions and poured with 100 ml of boiling water. After boiling, add melted internal pork fat to the broth. Cool the finished ointment and put it in the refrigerator.
- One more effective means in the fight against osteochondrosis is an ointment prepared from herbs such as marshmallow root, lavender, yarrow, horsetail, and dandelion root. All ingredients are taken equally and poured with boiling water; after boiling, add melted internal fat.
- To obtain this ointment for the treatment of cervical and thoracic osteochondrosis, you need to prepare the following herbs: burdock root, mint, plantain leaf, pine buds, chamomile flowers, tricolor violet herb. Further preparation is similar to the previous recipe.
A group of these drugs is intended to reduce pain, which is almost always present with osteochondrosis. Medicines also help remove swelling and improve blood circulation in problem areas.

Normal blood circulation is a very important point in the treatment of the spine. Taking medications allows you to improve the nutrition of the intervertebral discs, which helps to relieve the acute period more quickly.
- Eufillin. This drug has a wide range of effects. Being primarily a bronchodilator, it also improves blood circulation in the peripheral circle, thereby dilating the blood vessels of the muscles of the body and brain. The drug is also used in hardware therapy for local effects on the spine.
- Pentoxifylline. It has a local effect, dilating blood vessels in the problem area of the body, improving peripheral blood circulation.
- Vinpocetine. Prescribed in the acute period of cervical osteochondrosis, in case of impaired blood circulation in the brain, with migraine-like pain and other negative manifestations of the disease. It also has neuroprotective and antihypoxic effects.
Muscle relaxants
This group of drugs allows you to quickly relieve muscle-tonic syndrome, which helps improve blood circulation, relieve pain and swelling.
- Mydocalm. This drug has a selective effect on the body, relieving muscle spasm and tension, but without inhibiting nerve impulses for the normal functioning of the muscular skeleton. It is well tolerated, improves blood circulation and has an analgesic effect. Contraindicated if you are allergic to lidocaine and tolperisone.
- Tizanidine. This drug effectively relieves muscle spasms and helps increase strength during movement. Does not inhibit impulse transmission. Relieves muscle spasticity, reduces pain when moving. Side effects: drowsiness, fatigue, lethargy. The drug is contraindicated during pregnancy and kidney disease.
Blockades
When a hernia or protrusion appears that puts pressure on the nerve roots, causing pain and other symptoms, blockades are used.

Blockades are introduced into various locations: into the pinched nerve, near the root, into the deep layers of muscles near the spine or under the skin. For blockades, Novocaine, Lidocaine or the hormone Diprospan are used. In most cases, blockades immediately relieve pain, and hormonal injections additionally neutralize swelling. Treatment with blockades is carried out 4-5 times at equal intervals.
B vitamins are always included in the treatment regimen for cervical osteochondrosis. This is due to the fact that the active substances help reduce inflammation, strengthen muscles, and suppress negative neurological symptoms.
- Neurovitan.
- Milgamma.
- Pentovit.
Chondroprotectors
Chondroprotectors are drugs that, over time, restore and strengthen the cartilage tissue that makes up the intervertebral discs. There are several types of drugs according to the method of use:
- Tablets and capsules.
- Injections.
- Ointments.
The most popular include Dona, Structum, Alflutop.
Anti-inflammatory tablets play a very important role in the treatment of osteochondrosis, since this disease is accompanied by the destruction of bone tissue and intervertebral ligaments and joints, which is accompanied by a strong inflammatory process and tissue swelling.
Non-steroidal anti-inflammatory drugs, acting on various substances, suppress pain sensitivity. This group of drugs not only relieves pain, but also reduces fever, relieves inflammation and swelling.
Among the most popular anti-inflammatory tablets for osteochondrosis, it is worth highlighting:
- Diclofenac.
- Voltaren.
- Aspirin.
- Butadion.
- Indomethacin.
- Nimesulide.
- Ketoprofen.
Diclofenac
A popular non-steroidal anti-inflammatory drug that contains the active component diclofenac sodium. It not only has an anti-inflammatory effect, but also relieves pain and fever.
The dosage is prescribed by the attending physician, but adult patients usually take 25-50 mg two to three times every 24 hours. Do not chew the tablets and take them with meals. Once a therapeutic effect is achieved, the dose should be gradually reduced. The maintenance dosage is 50 mg per 24 hours.
READ ALSO: Violation of venous outflow in cervical osteochondrosis
Patients with a high risk of developing gastric bleeding, erosions and ulcers, aspirin-induced asthma, hematopoietic disorders, hemophilia, or intolerance to diclofenac are prohibited from taking the drug. For the treatment of pregnant women, children (up to six years of age), women who are breastfeeding breast milk, not used.
In some cases, use may cause abdominal pain, diarrhea, constipation, jaundice, vomiting, liver necrosis, hepatitis, colitis, loss of appetite, cirrhosis, headaches, drowsiness, irritation, fear, tinnitus, diplopia, scotoma.
Voltaren
Non-steroidal anti-inflammatory drug based on diclofenac sodium. It has anti-inflammatory, antipyretic and analgesic effects.
The dosage is individual, but doctors recommend taking the minimum effective dose. The standard dose is 100-150 mg per 24 hours. The tablets should be swallowed and washed down with plenty of liquid.
Patients with stomach ulcers, inflammatory bowel diseases, bronchial asthma, renal or liver failure, coronary artery bypass surgery, or intolerance to diclofenac are prohibited from taking the drug. Not prescribed for the treatment of pregnant women.
In some cases, use may be accompanied by nausea, abdominal pain, colitis, gastritis, vertigo, diplopia, headaches, cramps, and allergies.
Aspirin
A popular remedy that is taken for osteochondrosis to relieve inflammation. The medicine contains acetylsalicylic acid. It has an antipyretic and analgesic effect. Inhibits cyclooxygenase enzymes, which take part in the synthesis of protaglandins.
The most effective drugs
The effect of medicinal substances on the body is purely individual, so the same pills will have different effects on different people. There is no drug that is equally effective for every person.
The most effective drugs are those that affect the cause of the disease. In the case of osteochondrosis, these are tablets that reduce the rate of destruction of intervertebral discs. These include drugs that improve the nutrition of vertebral joints (pentoxifylline, aminophylline) and vitamin-mineral complexes.

Osteochondrosis cannot be overcome with drug therapy alone. Treatment must include rational physical activity, massage and various methods of physiotherapy.
For those people who want to forget about the unpleasant manifestations of osteochondrosis of the cervical or thoracic region, it is necessary to begin performing exercises that strengthen and give flexibility to the spine. While in a sitting position, you need to monitor your posture all the time and sleep on a hard mattress.
If you use a soft bed to sleep, the intervertebral discs are warmed, as a result of which they become easily shifted. Every day you should strengthen the muscles of the cervical, lumbar and thoracic back, and avoid a monotonous position of the spine.
For those who want to avoid physical suffering, you can use the following folk remedy for cervical osteochondrosis:
- Take a regular rolling pin for rolling out the dough in your right hand.
- Carefully and slowly, tap her on the right side of her shoulder, shoulder blade, and spine.
- Perform all the steps in the same way, but with the left side.
- You can perform this exercise at home, for example, while watching TV. Regular exercise will help you achieve maximum effect and eliminate the unpleasant manifestations of cervical and thoracic osteochondrosis.
Using the same rolling pin, you can do another effective exercise:
- Take a lying position on the floor.
- Roll the rolling pin on your back for about 15–20 minutes.
- It will be difficult to repeat the procedure the next day due to pain, but this is how it should be.
A rational combination of medications will best help with cervical osteochondrosis. That is, each of them must influence some link in the pathological process, thus enhancing the effect of each other.
An example of a rational treatment regimen:
- celecoxib – eliminates inflammation and relieves pain;
- baclofen – will relieve muscle spasms, thereby enhancing the analgesic effect;
- trental – improves blood circulation in the brain;
- milgamma - will accelerate the recovery of an unequal root;
- arthra - restores tissue of the intervertebral disc.

Medicines that cure osteochondrosis forever have not yet been invented, but there are medicines that stop pathological processes, restore previous activity, the joy of movement, and relieve pain.
The patient's health condition will begin to improve rapidly if the medications are chosen correctly. Tablets for osteochondrosis are the most effective, helping to neutralize spasms and relax muscle tissue.
Maintenance therapy uses antispasmodics and muscle relaxants. What pills to take for osteochondrosis are prescribed by a specialist after an examination. Drugs for the treatment of osteochondrosis are available in several formats; choose the one that is more convenient to use: injection, ointment, tablets.
Mydocalm is a drug whose effect reduces muscle spasms in the spinal and vertebral regions and has an analgesic effect. Available in the form of injections and tablets. The remedy for osteochondrosis does not cause muscle weakness and there is no sedative effect.
Sirdalud - dosed at 0.006 g per day, with use the volume increases to 0.01 g per day. The appointment time is calculated based on pain and muscle spasms;
Baclofen is a rarely prescribed drug. Dose: 0.005 g three times a day. The amount of medication is analyzed over time, increasing to 0.03-0.075 g for an adult. The time of use is prescribed by the doctor, based on severe symptoms. The drug is withdrawn gradually.
Katadolon is a drug that should be discussed separately. These tablets for osteochondrosis have a specific non-narcotic analgesic effect. The drug has an effect, activates K channels of neurons, acts on central system, relieves pain in the muscles of the spinal region, because

It is used in monotherapy and as a medicine for osteochondrosis in case of contraindication to non-steroidal anti-inflammatory drugs. The drug is prohibited for car drivers and pregnant and breastfeeding women.
How to cure cervical osteochondrosis at home? The answer is simple - do physical therapy every day.
Before going further, I’ll tell you when you can do exercise therapy. In the acute phase of osteochondrosis, physical therapy is contraindicated. The ideal time to start performing a set of exercises is immediately after pain and inflammation are eliminated, but not before.
Advantages of exercise therapy:
- improving the condition of the muscle corset;
- pain reduction;
- restoration of normal neck movement;
- reduction of muscle spasms;
- reduction of dizziness attacks;
- significant improvement in blood microcirculation in the cervical region;
- restoration of vertebral mobility.
Sounds good, doesn't it? What's the catch? The point is that you can’t skip classes, otherwise you won’t see the benefit.
Doing the exercises is not at all difficult, and the benefits are endless. The main thing is to do gymnastics regularly, or even better, every day, throughout your life. I assure you - there will be much less back problems.
Excellent article on the topic: Top 22 effective complex exercises for cervical osteochondrosis
Before you start reading the exercises, it is strongly recommended to remember the following rules:
- The pace is smooth, calm, without sudden movements. Otherwise, the risk of injury increases.
- Jerks must be avoided, otherwise dizziness and darkening of the eyes may occur.
- If you have acute pain in the neck, exercises are prohibited.
- The intensity of exercise should be increased gradually.
- It is advisable to perform a set of exercises every day at the same time. If desired, you can perform the exercises 2-3 times a day.
Anti-inflammatory tablets for osteochondrosis
Osteochondrosis of the spine occurs with the following pathological manifestations:
- backache;
- headache;
- disturbance of sensitivity (goosebumps, numbness of the skin);
- pain in the limbs;
- dizziness.

The pain syndrome is most pronounced during an exacerbation of the disease; during the lull period, the pain is either absent or has a weak aching character.
It can radiate to the leg, arm, and simulate heart and stomach diseases. The pain spreads along the affected nerve fiber. To eliminate pain, the doctor will prescribe anti-inflammatory drugs, analgesics and muscle relaxants.
Osteochondrosis of the cervical spine often leads to compression of the vertebral arteries, which supply blood to the brain. As a result, headaches and dizziness occur due to insufficient oxygen supply to the nerve cells. To treat cerebral ischemia, vasodilators and antispasmodics are prescribed.
In case of paresthesia (impaired skin sensitivity) in the form of goosebumps, numbness, tingling, the doctor prescribes B vitamins.
One of the mechanisms of pain in osteochondrosis is an inflammatory reaction at the site of a damaged disc and a pinched nerve root. Swelling develops around the tissues, which leads to compression of the pain receptors in them.
Anti-inflammatory drugs interrupt the development of pathological inflammation, thereby eliminating pain.
For osteochondrosis use:
- Diclofenac - prevents the development of an inflammatory reaction. The medicine is drunk either during a meal or immediately after it. It should be swallowed whole and washed down with a small amount of water. Diclofenac provokes the formation of ulcers in the stomach and duodenum, so omeprazole is prescribed along with it.
- Dolobid – has a powerful anti-inflammatory effect, the analgesic effect develops within an hour after administration.
- Lornoxicam - has an additional analgesic effect by disrupting the formation of pain impulses and weakening their perception in the brain. Copes well with chronic pain syndrome.
- Meloxicam does not provoke the formation of ulcerative defects on the mucous membrane of the digestive tract, so it is not contraindicated for stomach ulcers.
- Ibuprofen has a moderate anti-inflammatory effect, but it is suitable for long-term treatment as it rarely causes side effects.
- Naproxen - the anti-inflammatory effect develops over a month and is long-lasting and persistent. He rarely calls adverse reactions and additionally inhibits the process of degeneration (destruction) of cartilage tissue.
- This is a disease with a chronic, non-inflammatory nature. Arthrosis is characterized by cartilage degeneration with changes in the bones of the affected joint and symptoms of synovitis. As the disease progresses, there is a decrease in mobility in the joint up to complete immobility due to fusion of the articular ends of the bone joints.
Among all joint diseases, arthrosis occupies a leading position (60%). The frequency of cases with arthrosis correlates with age. People over 45 years of age suffer from this disease in approximately 13.9% of cases. There is a dependence on gender. In women, the incidence of arthrosis is 2 times higher than in men. The risk is also higher in people with excess body weight above the established norm (various degrees of obesity) and with congenital disorders of the musculoskeletal system.
The causes of this disease remain unknown to this day. Only predisposing factors are identified that can serve as an impetus for the development of arthrosis.
These factors are considered discrepancy between the load on a joint and its ability to resist this load. This occurs during heavy physical work, especially when the same joints are constantly involved in the work. This cause is also aggravated by possible obesity, which causes pressure on the joints to steadily increase.
Cases accompanied by a deficiency of joint nutrition, such as metabolic disorders in the body, changes in the functioning of organs, impaired blood supply to the joint, aggravate existing changes in the joints.
Types of arthrosis
Diagnosis primary (idiopathic) arthrosis is put in case of exclusion of all possible causes of development.
Secondary develops for the following reasons:
- Injury;
- Congenital developmental disorders of the musculoskeletal system;
- Endocrine diseases (obesity, diabetes);
- Metabolic disorders (gout, hemochromatosis);
- Changes in static-dynamic balance (flat feet, curvature of the spine);
- Chronic hemarthrosis.

Primary arthrosis is divided into 2 main clinical forms:
- Local arthrosis (1-2 joints);
- Generalized arthrosis (3 or more).
In the acute form of arthrosis, all the symptoms of the disease appear much stronger and last longer: the pain is unbearable, if the synovial membrane is involved, then a local increase in temperature and redness of the skin area appears. In the chronic form, the disease is long-term, sluggish, with occasional periods of exacerbation.
According to ICD-10, arthrosis refers to diseases of the musculoskeletal system and occupies an entire block called “Arthropathy”. In this block, the disease is divided into smaller components according to the location and degree of damage: polyarthrosis (3 or more joints are affected), coxarthrosis (hip joint), gonarthrosis (knee joint), etc.

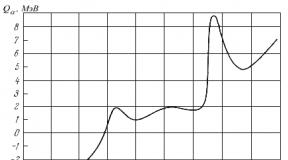
Symptoms
The main and most important diagnostic symptom (especially at the initial stage of the disease) is a feeling of soreness or pain in the joints, usually of a mechanical nature, i.e. related to movement. It appears at the end of the day, in the evening, after heavy physical work in the joint, its excessive activity during the day, and disappears when the joints are at rest.
Patients note increased pain when going down the stairs. Patients often complain of pain at the beginning of movement, the so-called starting pains. As you continue to move, the discomfort goes away. This is associated with stagnation of blood in the tissues surrounding the joint; when performing movements, circulation improves and, accordingly, all manifestations disappear.

Any prolonged pain is accompanied by muscle spasm, the same effect occurs when affected by arthrosis - the muscles around the joint are in a state of contraction, and the pain syndrome becomes more pronounced. When nerve fibers are involved in the pathological process, signs of radicular pain appear.
In the initial stages of the disease, pain appears occasionally after excessive stress on the joint and quickly disappears when it stops. But as arthrosis progresses, the pain becomes more intense, its duration increases, and its relief is worse. Therefore, it is necessary to suspect the symptoms of incipient arthrosis in the early stages of development and prescribe adequate treatment, otherwise the risk of disability is high.
Another important symptom of arthrosis is morning stiffness. It lasts no more than 30 minutes and develops both after daytime and after night rest.

Thus, when the joints of the back are affected, patients complain of pain and limited movement in the lumbar and back area, inability to straighten up after sleep and rest. It is often difficult for them to find a comfortable position in bed, so these patients take a long time to fall asleep. Involvement of the hand joints may also be accompanied by stiffness. When the joints of the lower limb are involved, the gait changes. It is difficult for them to go down stairs, every movement is accompanied by pain and stiffness. Crepitation and crunching accompany other symptoms of arthrosis.
If the synovial membrane is involved in the process with the development of inflammation, then a symptom such as synovitis appears.

Diagnosis of arthrosis
- Doctor treating arthrosis - rheumatologist– will begin his work with a survey in which he will find out the time of the first symptoms and which joints are affected.
- Before determining how to treat arthrosis in a patient, he will collect a family history, in which he will recognize the presence of similar symptoms in relatives.
- Next, he will examine and palpate the affected joints and prescribe tests, such as x-rays. An x-ray will determine possible narrowing of the joint space, the presence of bone growths, and areas of ossification of the joint capsule (ossification).
- The doctor will then make a diagnosis that reflects the group ( primary or secondary), the affected joint or joints, the degree of dysfunction in them and the stage ( acute or chronic). If the patient came in during an exacerbation, then this is also indicated in the diagnosis.

You can contact a rheumatologist either by registration or by a specialist from a private clinic at any diagnostic center. It is impossible to say exactly where it is better to receive treatment, because it is not always where it costs more and the quality is better than free medical care. Everything depends on the skills and abilities of the specialist, and it is extremely difficult to determine this by “cost”.
Treatment
Treatment of arthrosis begins with a correct diagnosis. To avoid asking questions “What’s wrong with my joints?”, “How can I cure it?” you need to immediately consult a doctor for help. After receiving all the necessary data, the doctor will decide which drugs and which procedures are suitable for this particular patient, take into account all his concomitant diseases and general condition and prescribe the most effective treatment- drugs, exercises, physiotherapy and other modern methods.
For almost any diagnosis, two treatment options are possible: medicinal and non-medicinal.
Drug therapy consists of the following groups of drugs:
- Non-steroidal anti-inflammatory drugs (NSAIDs). Reduce inflammation in the periarticular areas with the development of an analgesic effect. Of these drugs, preference is given to Ibuprofen, Diclofenac, Voltaren, Fenoprofen, Meloxicam.
- If it is impossible to take NSAIDs, use intra-articular injection of corticosteroids(Diprospan, Kenalog). They suppress certain intracellular mechanisms, reduce the level of phospholipase A2 and interleukin 1, which lead to the destruction of cartilage tissue. Corticosteroids are prescribed for symptoms of synovitis. These drugs can be administered to one joint no more than 4 times a year.
- Chondroprotectors. They have protective properties, preventing damage and destruction of cartilage. The drugs of choice are Artron, Arteparon, Rumalon.
- It is possible to insert an artificial synovial fluid based on hyaluronic acid preparations (Duralan, Giastat, etc.). Such drugs slow down the destruction of cartilage.
- If the process extends to the periarticular tissues, then an important step in the treatment of arthrosis will be the prescription of medications, reducing venous stasis and improving microcirculation: Trental, Nicotinic acid, Nifedipine.
- If the muscle spasm is strong enough, you can take muscle relaxants- Sirdalud, Mydocalm.
- With a pronounced limitation of joint mobility, the development of muscle stiffness, the question arises about surgical intervention(Osteotomy, Joint endoprosthetics).

Arthrosis is a collective concept denoting degenerative processes occurring in the joint. There are many types of arthrosis, differing in the cause of development, symptoms, treatment methods and outcomes. Degenerative processes are often preceded by inflammation or injury. Arthrosis can occur at any age, but more often the disease affects women over 40 years of age.
Classification
The classification of arthrosis is based on the cause of joint pathology. The following types of arthrosis are distinguished:
- Psoriatic arthrosis;
- Gouty arthrosis;
- Reactive arthrosis;
- Osteoarthritis.
Each type of disease has several degrees of development, depending on the severity of the pathological process. Accordingly, treatment approaches differ. If it is impossible to determine the cause of the pathological process in the joint, they speak of idiopathic arthrosis.
The classification also takes into account the localization of the pathological process:
- Damage to the hip joint – coxarthrosis;
- Damage to the toes.
Large joints of the legs are most often affected.
If signs of articular pathology appear, it is necessary to consult a doctor to establish the correct diagnosis, since different types of pathologies need to be treated differently.
Principles of diagnosis and treatment
To diagnose any type of arthrosis, the following methods are used:
- Identification of active and passive complaints;
- Study of the dynamics of the disease;
- Inspection and palpation of the affected joint;
- Radiography;
- Arthroscopy;
- Study of joint fluid.
Treatment is carried out in a conservative way - taking medications, physiotherapy, massage and therapeutic exercises. For severe deformity, surgical treatment is indicated. Each type of arthrosis has its own characteristics in diagnosis and treatment.
Psoriatic
This type of pathology is one of the symptoms of psoriasis. Typically, joint damage develops in patients who have suffered from skin rashes for a long time. Psoriatic arthrosis usually affects large joints - hip, knee, ankle, and less commonly the toes.
Symptoms of the disease are caused by the inflammatory process. Morning stiffness is characteristic, which can reach such a degree that the patient becomes immobilized. The pain syndrome is quite pronounced; the patient describes the pain as aching and pulling. In the acute phase, swelling and redness of the skin over the joint is noted, it becomes hot to the touch. Psoriasis is characterized by asymmetric joint damage.
The presence of skin rashes is important in diagnosis. However, it should be remembered that rashes are not always observed simultaneously with joint damage. Laboratory diagnostics do not have specific indicators. Certain features are present in x-ray examination:
- Osteoporosis;
- Periarticular erosions;
- Periostitis - bone growths along the edges of the joint;
- When the toes are affected, there is a consistent change between the phalanges of one finger.
Depending on the number of affected joints, the severity of the disease is determined.
Treatment is carried out conservatively:
- NSAIDs (non-steroidal anti-inflammatory drugs) - Ibuprofen, Airtal are prescribed for several months;
- Intra-articular administration of glucocorticoids;
- Sulfasalazine is prescribed for long-term use;
- In severe cases of the disease, cytostatics are indicated.
In addition to medications, physiotherapy includes phototherapy and electrophoresis with glucocorticoids. A mandatory component of treatment is gymnastics. In consultation with the attending physician, traditional treatment is used.
If conservative therapy is ineffective and severe joint deformation occurs, surgical treatment is indicated - endoprosthetics, arthroplasty.
Gouty
Arthrosis develops due to a violation of the metabolism of uric acid in the body. Urea salts are deposited in the joints, causing inflammation and subsequent deformation. The interphalangeal joints of the feet are most often affected.
The disease is characterized by a chronic course with periodic exacerbations. Joint syndrome presented with moderate pain, swelling and swelling of the joint.
A specific sign of gout are. These are accumulations of uric acid salts in soft tissues - in the ears, on the extensor surfaces of the limbs.
With a long course of the disease, gout nodes form at the site of the tophi. These are large formations, when opened, a white curdled mass formed by urea salts is released.
To diagnose gouty arthrosis, a study of the level of uric acid in the blood is used. Radiological signs of gout include:
- Compaction of soft tissues;
- Focal darkening in the joint area;
- Periarticular erosions.
Treatment is carried out using conservative methods. A diet aimed at reducing the level of uric acid in the body is of great importance. Patients are advised to exclude from the diet:
- Fatty meats and fish;
- Smoked meats, meat and fish delicacies;
- Canned foods;
- Sorrel;
- Legumes;
- Chocolate;
- Strong tea, coffee, alcohol.
The main drug for the treatment of gout is. Patients take this medicine for life. To relieve pain, gels and ointments with NSAIDs are prescribed. Physiotherapy has a good effect - paraffin applications, diadynamic currents, therapeutic baths.
Rheumatoid
The disease has a hereditary predisposition. It develops as allergic arthrosis, which is based on an autoimmune reaction. Any joints of the legs are subject to a pathological process. The disease is characterized by chronic inflammation and persistent deformation of the joints, leading to loss of mobility.
Arthrosis is characterized by intense pain and morning stiffness. The duration of morning stiffness is at least 30 minutes - this is a diagnostic sign of the disease. The pain reaches its maximum in the evening. There is swelling and redness of the joint.
Diagnostic criteria are the detection of rheumatoid factor and specific radiographic changes. There are four radiographic stages of arthrosis:
- The changes are minimal, a slight narrowing of the joint space is noted;
- Single erosions appear along the edges of the crack;
- There are more erosions, a significant narrowing of the joint space;
- The joint space is practically absent, there is a large number of erosions.
Several groups of drugs are used for treatment. They are prescribed sequentially - if drugs from one group are ineffective, they move on to the next:
- NSAIDs – Movalis, Nimika;
- Glucocorticoids – Metipred, Diprospan;
- Cytostatics – Methotrexate;
- Sulfasalazine;
- Gold preparations – Tauredon, Krizanol;
- Monoclonal antibodies - Arava.
If persistent deformity occurs, surgical treatment is indicated. The rheumatoid process is the most progressive arthrosis, quickly leading to irreversible deformation.
Reactive
This is an infectious arthrosis caused by the presence of chlamydia, mycoplasma, and E. coli in the body. The joint is not affected by these bacteria, but by antibodies that are produced in response to their presence.
Infectious arthrosis is characterized by moderate pain and severe signs of inflammation of the joint. The knee is most often affected - it becomes swollen, the skin over it turns red, and the local temperature rises. Due to pain and swelling, movement in the knee is limited. Sometimes observed general signs intoxication.
Diagnosis is based on history, clinical examination and examination of joint fluid. X-ray examination does not reveal specific changes.
Treatment is carried out conservatively. Drug therapy is prescribed that affects the infectious factor and eliminates the inflammatory process:
- Antibiotics from the group of macrolides or tetracyclines;
- Non-steroidal anti-inflammatory drugs;
- Analgesics;
- Means for improving microcirculation.
Physiotherapeutic methods are used - UHF, electrophoresis. This process can be considered pseudarthrosis, since truly degenerative changes do not occur.
Post-traumatic
Develops after joint injury. Inadequate or incomplete treatment leads to chronicity of the inflammatory process and degenerative changes in cartilage tissue. Large joints are most often affected.
The disease is characterized by moderate pain, intensifying in the evening. Signs of inflammation are usually not observed. The long course of the disease leads to the formation of joint deformities.
A history of trauma is important for diagnosis. X-ray changes are nonspecific; signs of a fracture in the joint area can be detected.
Treatment is carried out symptomatically - painkillers, non-steroidal anti-inflammatory drugs, and chondroprotectors are prescribed.
Osteoarthritis
This leads to severe dysfunction of the joint. The basis of the pathological process is degeneration of articular cartilage. The main thing is pain. It occurs immediately after waking up, continues throughout the day and intensifies in the evening. Patients note limited movement and crunching in the joints.
The diagnosis is established on the basis of x-ray examination:
- Narrowing of the joint space;
- Formation of osteophytes - bone growths;
- Bone compaction – osteosclerosis.
Treatment is carried out using conservative and surgical methods.
Arthrosis is a large group of diseases characterized by the destruction of cartilage tissue of joints and disruption of their functions. They arise for various reasons. A common symptom is pain and joint deformation of varying severity. Depending on the type of arthrosis, treatment tactics and prognosis are determined.
Arthritis and arthrosis are diseases that affect the joints. There are many varieties of these pathologies. If we consider arthrosis, then gradual age-related deformation of joints is divided into types depending on which particular human joints are affected by the pathological process:
Inflammation of the knees (gonarthrosis), cervical deformity (uncovertebral arthrosis), diseases of the hip joint (coxarthrosis), problems of the shoulder joint, primary polyosteoarthrosis, lesions of the ankle joint, diseases of the spine (spondyloarthrosis) are common.
Arthrosis develops in adulthood. They usually affect people over 40 years of age.
There are also several types of arthritis today. The disease, unlike arthrosis, affects younger patients.
Causes of arthrosis
Among the main preconditions that result in the development of arthrosis, special mention should be made of the natural aging of the body. With age, the cartilage tissue covering the surfaces of the joints loses its elasticity and loses its natural resistance to stress.
It is important to note that aging will not always be the onset of arthrosis. The immediate impetus for the development of the problem will be the resulting mechanical injuries. An excessive degree of mobility of individual parts of the joint can also lead to arthrosis.
In addition to the above reasons, arthrosis is provoked by a person’s professional activity if it is associated with increased stress. For example, arthrosis of the knee joint is a common diagnosis among miners.
This chronic disease is characterized by changes that occur in the articulating joints that make up the bones. If at the very beginning of arthrosis pain can occur only in the inner area of the bursa, then soon, if there is no appropriate treatment, pain occurs in the cartilage covering the surface of the bones. Gradually this happens:
- softening of cartilage on bone;
- its destruction.
Moreover, along with this pathological process, a significant compaction of bone tissue is observed, which causes the formation of osteophytes (bone growths).
Main types of arthrosis
The changes that occur during the development of arthrosis affect only the joints. Most often they suffer from arthrosis of the knee joint, because it is this part of the leg that is most vulnerable. Typically, gonarthrosis of the knee joint affects older people. The pathological process covers the knee joint area on both legs, but only one of them can hurt.
With coxarthrosis, the most severe type of arthrosis that develops in middle-aged and elderly people, the patient experiences severe, sometimes excruciating pain in the pelvic area. It is characteristic that women suffer much more often, and their pathology is more pronounced.
Uncovertebral arthrosis directly depends on the patient’s age: the older he is, the higher the chance of getting sick. This pattern is explained by the fact that over time the following is observed:
- loss of the former natural elasticity of cartilage;
- gradual decrease in the volume of synovial fluid in the joints.
Shoulder arthrosis is no less common among our compatriots, but its treatment process is much easier and faster when compared with other groups of diseases. Pathology develops in older people.
Women are characterized by osteoarthritis of the hands, and it progresses after menopause. Signs of a problem will be:
- burning in the joints;
- tingling in fingers;
- decreased hand mobility.
 If the ankle joint is affected, this occurs after injuries, dislocations, sprains and bruises of the foot ligaments. The causes of the disease can be diabetes mellitus, gouty arthritis, dysplasia and rheumatoid arthritis.
If the ankle joint is affected, this occurs after injuries, dislocations, sprains and bruises of the foot ligaments. The causes of the disease can be diabetes mellitus, gouty arthritis, dysplasia and rheumatoid arthritis.
Spinal diseases are a separate group of arthrosis, in which the cartilage tissue of the spinal column is damaged. This provokes various overloads in its departments.
When a person suffers from weakening of articular ligaments and muscle dystrophy, then we are talking about primary polyosteoarthrosis. This type of disease develops in women during menopause and is explained by hormonal changes in the female body. The disease usually manifests itself as tendonopathy (damage to the tendon at the site of attachment to the bone) and discopathy (wear of the intervertebral discs).
The inflammatory process in arthritis of the knee joint is usually accompanied by:
- swelling of the joints;
- redness;
- severe pain syndrome.
The pain does not stop even at rest and after a long rest. In some situations, the pain even intensifies.
The occurrence of arthrosis of the knee joint, elbow, and hip is associated with the development of inflammation in the patient’s body, hormonal disorders or excessive activity of the immune system, which, due to an error, directs all its work to actively fight against its own body.
Arthritis and polyarthritis
Arthritis is characterized by an inflammatory process in one joint or several at once. When arthritis affects two or more joints, the condition is called polyarthritis.
Doctors distinguish several types of disease, depending on what exactly its prerequisites are:
- rheumatoid;
- infectious;
- reactive;
- exchange;
- psoriatic.
The signs that appear as the pathology progresses largely depend on its cause. Common symptoms of arthritis will be pain in the joints, especially when the weather changes, swelling, increased overall body temperature, and decreased appetite.
If polyarthritis of an infectious nature develops, then redness of the skin over the diseased joint, limited mobility and swelling may be observed. With the rheumatoid form of the disease, the patient will notice a significant increase in temperature and pain in the internal organs.
Types of polyarthritis
As for polyarthritis, not everything is clear with it either. Rheumatoid polyarthritis is associated with the penetration of infections into the cavity of the joint capsule. This type of disease provokes the development of chronic damage in several joints, for example, inflammation of the knee and ankle joint.
The disease is extremely difficult to treat, especially if it is advanced. As a result of the disease, damage to the connective tissues of the joint occurs.
Infectious polyarthritis covers the joints following the transferred organism infectious disease. Provided timely and high-quality treatment, getting rid of it will not be difficult, however, there are exceptions. If therapy is ignored, the normal functioning of the knee joint and the entire body is disrupted.
The metabolic type of polyarthritis is a condition that arose against the background of disruptions in metabolic processes. The main reason for the problem is the accumulation of salts (urates) in the joints, for example, lesions:
- knee;
- elbow joint;
- big toe.
Psoriatic inflammation in several joints can begin to bother a person even at an early age. Most often, the ankle and knee joint area are affected, and only six months after the first symptoms characteristic of the skin pathology psoriasis. The causes of psoriasis have not been fully studied by medicine at the moment. It is believed to be caused by problems with the immune system.
Reactive polyarthritis is distinguished by a special, peculiar reaction of the human body to infectious infections of internal organs (one or more). This variation of arthritis causes colitis, polyneuritis and conjunctivitis, which significantly complicates treatment.
- Etiological information
- Symptomatic picture
- Diagnostic measures
- Therapeutic complex
 Arthritis of the foot is a set of pathological conditions of inflammatory origin that affect the joints of the tarsal, metatarsal bones and phalanges of the foot.
Arthritis of the foot is a set of pathological conditions of inflammatory origin that affect the joints of the tarsal, metatarsal bones and phalanges of the foot.
Among all forms, rheumatoid, post-traumatic, gouty, and infectious are common. They have an acute or chronic onset. Damage to the joints of the foot is often combined with arthritis of the ankle and arthritis of the fingers of the lower extremity.
The human foot is the main component of the musculoskeletal system and is represented by a complex anatomical and functional structure that is subject to enormous dynamo-static loads.
Disorder of any function of the foot due to injury or pathology can lead to the formation of pathological processes in the articular joints of the spinal column, pelvis and the entire lower limb.
The bone formations of the foot are combined with the bones of the lower leg and with each other through the articular joints of the tarsometatarsus and phalanges. The articular joints of the posterior portion (tarsus) are the articulations of the talus, calcaneus, cuboid, sphenoid and navicular bones. The talonavicular and calcaneocuboid joints form the Chopart joint or the transverse articular joint of the tarsus.
The bone structures of the mid-anterior section are combined by the tarsometatarsal (Lisfranc), intermetatarsal, metatarsophalangeal and interphalangeal joints.
The pathological process can develop in each of the described joints. The joints of the posterior-middle section are characterized by low mobility in comparison with the articular joints of the anterior section.
Etiological information
Inflammatory phenomena in arterial joints can form primarily (as an independent unit) or as a result of infectious, metabolic, or autoimmune processes existing in the body. In etiology, a connection is often visualized with previous trauma to the joints or the bones themselves. Moreover, the intermediate period between injury and manifestation is quite long. In the case of an open fracture or injury, inflammatory phenomena can occur as a result of direct bacterial entry into the synovial zone. In some cases, the pathological process occurs against the background of long-term injury to articular joints (wearing uncomfortable shoes, sports activities, ballet).
In a number of variants, the infectious origin enters arterial joints through the lymphatic pathways from septic foci localized adjacent to the synovial cavity (with boils, erysipelas, osteomyelitis, infected wound surfaces, bites).
The reactive form, manifesting after a genitourinary or intestinal process of infectious etiology, is observed in Reiter's syndrome.
The disease is a pathology with an insufficiently established etiological factor. Destructive transformations are formed as a result of damage to the synovial layer of the cavity by IR formed in the body.
In arthritis against the background of gouty lesions, the pathological process is triggered by urate deposits in the articular cavity of the thumb.
Provoking factors are old age, excess body weight, intense physical activity, smoking, immunodeficiency states, impaired metabolic processes, etc., which, in fact, can aggravate the process, leading to arthrosis-arthritis of the foot.
Symptomatic picture
Regardless of location and etiology, there are a number of common clinical manifestations:
- pain sensation;
- change in the appearance of the articular joint;
- functioning disorder.
Along with this, each variety has its own specific characteristics. The pain sensation is characterized by constancy, intensifying when walking or standing for a long time and subsiding after rest. The gouty form is characterized by an attack-like pain sensation. The soft tissues over the damaged joints are swollen, the skin is hyperemic and hot to palpation. Dysfunction is represented by a decrease in foot mobility, a decrease in the volume and amplitude of motor acts. Loss of usual mobility can be caused by severe pain and an increase in the size of bone growths. It is often accompanied by a typical crunching or clicking sound.
Typical signs include:
- Stiffness in the morning. Patients usually complain that they cannot move around after prolonged sleep or lying down.
- Numerous joint damage.
- Characteristic deformities of the phalanges and feet.
- Painful sensations are added to limited mobility, which is why the gait changes, the patient begins to limp or cannot stand on his foot at all.
Arthritis of the foot (except for the post-traumatic type) is mainly a symptom of polyarthritis.
Diagnostic measures
 During the physical examination, an assessment is made of the position, shape of the foot, the nature of passive-active motor acts, palpation with temperature assessment; skin analysis, gait analysis, etc.
During the physical examination, an assessment is made of the position, shape of the foot, the nature of passive-active motor acts, palpation with temperature assessment; skin analysis, gait analysis, etc.
In diagnostic measures, the main role is given to x-ray examinations of the foot, ultrasound examination of articular joints, MRI and CT scans of distal areas of the lower limb. The following are used as additional studies:
- immunological analysis;
- biochemical blood test, paying attention to the level of CRP, RF, uric acid, sugar.
Diagnostic puncture of the small joints of the foot can help in identifying the infectious origin.
Therapeutic complex
The treatment complex consists of pathogenetic and symptomatic therapy, rehabilitation measures, and in severe cases, surgical intervention.
A prerequisite is to limit the load on the foot and avoid long-term injury. In the acute period, immobilization with a plaster splint and walking with crutches are prescribed.
A dietary approach is mainly necessary for the gouty form.
At different types Oral, parenteral and local NSAIDs are used.
In the case of an infectious etiology, antibiotic therapy is prescribed, and GCS is often administered intra-articularly.
During the rehabilitation period, chondroprotective agents, physiotherapeutic procedures, exercise therapy and massage are indicated.
Deforming arthrosis of the knee joint grades 1, 2, 3: causes, symptoms, treatment

Deforming arthrosis of the knee joint is a very common disease that can occur in both young and old people. The fact is that the knee is considered one of the most mobile and loaded parts of the support system. Over time, the tissue wears out, and pain and stiffness appear in the affected joint. Treatment of the disease should be mandatory.
Features of the pathology
Arthrosis of the knee joint is characterized by the development of degenerative and dystrophic processes within it. The cartilage tissue is gradually destroyed. Untimely treatment leads to joint deformation and inability to move normally. In addition, due to the destruction of cartilage, the body turns on the immune response and begins to grow bone tissue - osteophytes. This further limits the functionality of the knee.

This disease is constantly progressing. Its treatment is necessary in order to stop further deformation of the joint. If the therapy was incorrect or untimely, then arthrosis will deform the knee joint, after which it will no longer be possible to change anything.
Causes of pathology
So, deforming arthrosis of the knee can be provoked by completely different factors, but the risk group includes people with a hereditary predisposition to diseases of the supporting apparatus, and with excessive body weight. Too much weight aggravates the condition of the joints. Moreover, deforming arthrosis of the knee can be unilateral or bilateral.
The following reasons can provoke knee joint disease:
- Meniscus injuries, knee fractures, dislocations, damage to ligaments or other components of the joint. They contribute to the development of gonarthrosis in young people. The victim feels severe pain and cannot move his leg. If you do not begin to treat the injured joint immediately, the risk of developing early arthrosis increases several times.
- Removal of the meniscus due to surgery.

- Too much stress on the knee joint. It is better to avoid intense training in old age. This can provoke the appearance of microtraumas, which at first do not make themselves felt.
- Weakness of the ligamentous and muscular apparatus.
- Other diseases of the knee joint.
- Obesity. In this case, heavy weight increases pressure on the knee and contributes to the development of the disease, and also deforms the bones.
- Disturbance of metabolic processes in tissues. In this case, they do not learn the necessary elements for normal functioning well enough. The cartilage gradually begins to deteriorate, and the knee begins to deform.
- Frequent stress and nervous tension.
- Circulatory disorders.
These reasons cause defarthrosis even in youth. Naturally, treatment of all these pathological conditions will help to significantly slow down the development of the disease.
General symptoms and signs of the disease
The following symptoms are typical for deforming arthrosis of the knee joint:
- Pain extending to the lower leg.
- The discomfort becomes stronger when climbing stairs or after prolonged standing (walking).
- Stiffness in the affected knee.
- Swelling of the joint.

- When bending the knee, a crunching sound is heard in it.
- Morning stiffness of the joint lasts until the person moves away.
- The patient cannot fully bend or straighten the leg, as he feels severe pain.
- If the patient has early stage arthrosis of the knee, the pain syndrome disappears after a short rest and at rest.
Professor, Doctor of Medical Sciences Sergei Mikhailovich Bubnovsky tells how to distinguish the disease we are interested in from other similar ones in the program “About the Most Important Thing”:
It should be noted that each stage of the disease has its own symptoms. For example, the nature of the pain can be different:
- Morning pain goes away within 30-40 minutes.
- The inflammatory process provokes pain during certain movements.
- Unpleasant sensations that disturb sleep occur due to neuropathy or muscle spasm.
- Sudden severe pain due to pinching of the joint by muscles.
Each degree of knee joint disease is characterized by an intensification of the main manifestations.
Deforming arthrosis of the knee joint 1st degree: features of manifestation
Defarthrosis in this case is practically not noticed by the patient, since the symptoms and signs are practically not felt. Mild pain in the knee may only appear with intense movement. That is, the patient cannot yet suspect that he is developing arthrosis.
Even slight stiffness in the joint is not alarming. There is virtually no inflammation or acute onset of the disease. This stage is characterized by the accumulation of a small amount of synovial fluid, so the appearance of a Becker cyst is possible. However, most patients, even in this case, do not see a doctor.

Despite the fact that the cartilage is already undergoing pathological changes, they are not so serious as to deform the knee joint. At this stage of the disease, even X-ray examination does not always show any destruction. Therefore, additional instrumental diagnostic methods will be required.
Treatment of this stage of the disease is carried out not only with the help of anti-inflammatory drugs, but also with therapeutic exercises. Motor activity must be maintained so that the joint produces synovial fluid that nourishes cartilage and other tissues.
Associate Professor of the Department of Neurology and Manual Therapy of KSMA Olga Sergeevna Kochergina shares her knowledge about the disease:
Deforming arthrosis of the knee joint, grade 2
The second stage of arthrosis of the knee joint is characterized by increased pain, which sometimes impairs the ability to work, although the person can care for himself. This degree of gonarthrosis already forces a person to see a doctor.
The emerging symptoms disrupt the patient’s normal life, as the pain becomes almost constant and occurs with any even slight movement. It only calms down when at rest. It is especially difficult for the patient to take his first steps after waking up in the morning. Since at this stage of the disease the osteophytes grow quite strongly, this increases the discomfort. Sometimes the pain appears even at night, disrupting sleep. The man begins to limp.

The knee bends and straightens with difficulty, and swelling appears in the affected area. The muscles of the joint go into spasm. The second degree of gonarthrosis is characterized by the development of an inflammatory process. The limitation in mobility becomes very noticeable. The patient practically cannot walk without additional orthopedic devices.
Treatment of deforming arthrosis in this case is carried out using various methods: drug therapy, therapeutic massage and physical education, physiotherapeutic procedures. Complex cases require surgical intervention. Further development of the disease is fraught with disability.
Deforming gonarthrosis of the third degree: features of manifestation
The pain in the knee joint becomes constant and does not disappear even at rest. Moreover, the unpleasant sensations intensify even with a sudden change in weather. Characteristic of this degree is gait disturbance. The lameness becomes very noticeable.
Swelling of the knee joint lasts quite a long time and is significantly expressed. The deformation of the joint becomes noticeable. It takes on an X- or O-shape. The mobility of the leg is very limited, to the point that it does not bend or extend at all. Even small movements are accompanied by an unpleasant crunch.

In this case, the cartilage is destroyed very much. The x-ray shows a strong narrowing of the interarticular space. Inflammation provokes a large accumulation of fluid inside the joint. This degree of the disease is distinguished by the fact that all symptoms intensify several times. Often drug treatment here it is no longer effective; surgery is required to replace the knee joint with an artificial prosthesis.
Arthrosis cannot be completely cured. The degenerative process deforms the joint so much that the person may already become disabled.
In order for the doctor to prescribe effective treatment, the patient must be examined. It uses not only radiography, but also MRI, ultrasound, and arthroscopy of the knee joint, which can also serve as a treatment.
Leading researcher at the Institute of Rheumatology of the Russian Academy of Medical Sciences, Elena Sergeevna Tsvetkova, will share useful information with you about treatment and prevention:
Features of treatment of the disease
Despite the fact that arthrosis cannot be completely cured, it should not be left to chance. You should try to slow down the development of the disease, eliminate the symptoms and restore the functionality of the joint.
Medication therapy involves the use of the following means:
- Non-hormonal anti-inflammatory drugs: Ibuprofen, Indomethacin. They help eliminate pain and inflammation. Typically, NSAIDs are used before massage or exercise therapy is applied. But these medications are not able to treat arthrosis itself. They only relieve symptoms.
- Chondroprotectors: “Teraflex”, “Dona”. These medications are the basis of treatment, as they restore damaged cartilage and improve its nutrition. Naturally, they cannot completely cure the disease, but they are quite capable of improving the patient’s quality of life. Without chondroprotectors, treatment of knee arthrosis will be ineffective. There are practically no other ways to restore cartilage.
- Injectable corticosteroids that are injected directly into the joint: Hydrocortisone, Diprospan. They allow you to eliminate pain as quickly as possible, and for a long time. However, injections can only be given a few times a year.
- Drugs for dilating blood vessels that will prevent the formation of varicose nodes: “Xanatinol”, “Trental”. They make it possible to restore blood circulation in the joint.
- Hyaluronic acid injection once a year. It is effective only in the first and second stages of arthrosis development.
- Local painkillers.
Diet is considered part of complex treatment. It does not involve fasting or strict food restrictions. However, the diet should promote weight loss if necessary. That is, meals should be frequent and fractional. It is best to follow a diet that involves eating half of the foods raw. Naturally, you should give up alcohol and tobacco.

Physiotherapeutic treatment
The use of medications is only part of the therapy. It is complemented by physiotherapeutic procedures, therapeutic exercises, massage and even folk remedies. As for exercise therapy, most exercises are performed in a lying or sitting position so that the load on the knee joint is minimal.
The most popular exercises are:
- You should lie on your back, on the floor. The affected limb needs to be straightened and raised 20 cm above the floor. You should hold your leg in this position for as long as possible. This will make it possible to reduce symptoms and strengthen muscles.
- While sitting on a chair, the right or left limb needs to be extended forward. Next, the foot moves up and down.

- You should sit on a high pedestal and dangle your legs slightly. This exercise must be performed often and at a moderate pace.
- While lying down, you need to bend your knees and pull them towards your stomach.
Each exercise is repeated at least 5 times. Moreover, gymnastics for gonarthrosis must be done very carefully so that it does not cause discomfort.
Laser therapy is a useful physiotherapeutic procedure. It is often more effective than medications. The laser perfectly relieves the inflammatory process. Oxygen therapy has excellent reviews.
In the most difficult cases, surgical intervention is used. Knee arthrosis should be treated in this way only in extreme cases. The operation involves the removal of osteophytes, as well as complete replacement of the joint.
It will be effective to use shock wave therapy (SWT) when treating stages 2-3. How this process takes place at the medical center, watch the video:
Traditional treatment of pathology
Defarthrosis can also be treated with folk remedies. For example, the following recipes are considered useful:
- Compress made from horseradish root and blue clay. It should be applied to the right or left joint. Within a few hours the pain will go away.
- Dandelion tincture. It is used for rubbing, taken in the evening. This remedy perfectly relieves swelling.

- Celandine juice. It is used for compresses. Simply saturate the fabric with this liquid and apply it to the affected joint. Polyethylene is applied over the fabric. The procedure is repeated every day for at least a week. After this, you need to take a break for the same amount of time. The course of therapy must be repeated at least three times.
- Massage with honey. To begin with, the joints need to be steamed using a heating pad. Next, you need to apply honey to it and lightly rub it into the skin for 20 minutes. After completing the massage, apply a cabbage leaf to your knee and wrap it. A two-week course of such treatment will help the patient improve his condition.
An important step in the treatment of deforming knee arthrosis is sanatorium treatment. Here the patient will undergo a course of therapeutic aerobics and mineral baths. In addition, the treatment recommends the use of orthopedic devices that relieve the load on the damaged joint: canes, orthoses.
In any case, deforming arthrosis requires complex treatment. This will improve the patient's quality of life.
You can learn about the basics of exercise therapy for illness from this video.
Read also...
- Will I get married? Fortune telling online. Fortune telling for a new acquaintance. Fortune telling with playing cards Fortune telling by a friend
- Morozov Nikolay Aleksandrovich Nikolay Morozov Narodnaya Volya
- You can cook French fries in the microwave How to make your own French fries in the microwave
- Crispy pickled cucumbers in jars