Staphylococcus aureus in a 6-year-old child. Staphylococcus in children: causes, symptoms, treatment and consequences. Staphylococcus aureus in children. Forms of staphylococcal infection
The development of opportunistic microbes, which include staphylococcus, in the body of children is promoted by insufficiently strong immunity. The bacterium can infect various organs and cause serious and dangerous diseases. However, when staphylococcus is detected, it is not always necessary to urgently treat with antibiotics. It is much more important to restore the intestinal microflora so that beneficial bacteria can cope with the infection. It is important to take preventive measures to protect your child from exposure to harmful microorganisms.
Content:
General characteristics of staphylococcus
Staphylococci are bacteria that, under a microscope, look like tiny oval or round grains. They are grouped, forming “clusters” (“staphylococcus” translated from Greek means “clusters of grains”). There are many types of these bacteria. It was discovered that 14 species live in the human body, among which the following are dangerous: epidermal, saprophytic, hemolytic and Staphylococcus aureus.
The mechanism of their harmful effect on the body is associated with the presence of “pathogenicity factors” - the ability to release extremely toxic substances produced during their life activity. If a person’s immune defense is not strong enough (as, for example, in a child’s body), staphylococci penetrate into the blood, lymph, and body tissues. Here they secrete toxic enzymes, hemolysins (damaging blood cells - red blood cells, white blood cells and others) and many other extremely harmful substances. It is the presence large group toxic factors lead to a variety of diseases, such as sepsis, pneumonia, intestinal infection, meningitis and others.
Note: For comparison, it can be noted that the diphtheria bacillus, for example, secretes a single toxin and leads to the occurrence of only one disease.
The degree of danger of various types of staphylococci
The belonging of pathogenic staphylococci to a certain species is determined by the part of the body in which they primarily live. Accordingly, each species is the main causative agent of specific diseases.
Staphylococcus epidermidis
Lives in the skin and mucous membranes. If there are no wounds or damage, the bacterium is harmless to humans (even an infant), since beneficial microflora and immune cells easily neutralize its harmful effects. Most often, it poses a danger to people who have undergone surgery, as well as those who have wounds on the skin resulting from injuries. The most harmless consequence of exposure to staphylococcus is ulcers on the skin. Bacteria often affect the mucous membranes of the nose, throat and eyes. Penetrating into the body of children, staphylococcus can cause such severe pathologies as inflammation of the intracardiac mucous membrane (endocarditis) and blood poisoning.

Saprophytic staphylococcus
This bacterium rarely affects children. Exposure to saprophytic bacteria usually causes inflammation of the female genitourinary organs. For children, such bacteria are the most harmless. The resulting disease, as a rule, is quickly and easily cured within a few days.
Hemolytic staphylococcus
Prone to hemolysis, that is, destruction of blood cells. This type of bacterium affects the mucous membranes of the respiratory system and throat. As a result, purulent inflammatory processes occur in them (tonsillitis, tonsillitis, sinusitis). Complications may include otitis media, inflammation of the lymph nodes, and scarlet fever. This type of microbe is extremely resistant to antibiotics and easily spreads through blood vessels to any other organs.
Staphylococcus aureus
The pathogenicity of this type of bacterium is the highest. If staphylococci of other species secrete only some toxins, then this species is capable of secreting them in full, damaging the cells of a wide variety of organs. Bacteria of this species are resistant to most antibiotics. They are able to develop quickly in the body in both infants and adults.
Under a microscope, you can see that the bacterium is colored orange, which is why it was given this name. The microbe is extremely stable in the external environment. It can remain viable for a long time under the rays of the sun, withstands drying and heating up to a temperature of 150°. It is not killed by such strong disinfectants as ethyl alcohol and hydrogen peroxide. On the contrary, treatment with peroxide serves him well, since the released oxygen feeds him.
However, effective antiseptics that kill staphylococcal bacteria still exist. This is the usual “green stuff”, as well as “methylene blue” - substances from the group of organic dyes, aqueous solutions of which are used to disinfect and anesthetize wounds.
Video: Features of the development of staphylococcal infection
Causes of staphylococcal infection
In principle, staphylococci (including aureus) are classified as opportunistic microbes. They are present in a healthy body in a certain amount, without causing harm. The child constantly encounters bacteria found on household items, toys, clothes, and food.
The immune system of even a newborn baby can protect him from the disease. But if for some reason the immune system weakens, the infection begins to multiply quickly. Exceeding the norm of its content leads to the occurrence of numerous diseases. For example, factors contributing to the activation of staphylococci in the body in infants are:
- weakened immunity in the expectant mother during pregnancy if she had an infectious disease and was treated with antibiotics or if she took hormonal medications;
- underdevelopment of the immune system in premature infants or those with developmental defects;
- decreased resistance to infection in a formula-fed baby who is bottle-fed with formula.
Bacteria can enter an infant's body if they are in the mother's milk or if she has an inflammatory disease of the mammary glands. However, in breast milk staphylococcus also enters from the outside, from the surface healthy skin. If a nursing woman has no symptoms of the disease, and the content of staphylococcus in milk is acceptable, breastfeeding is not stopped.
Children of any age experience a weakening of the body's defenses after colds, intestinal infections and other diseases, as well as as a result of taking antibiotics. The development of staphylococcus in children is facilitated by insufficient care from adults and the child’s failure to comply with hygiene rules.
The cause of the disease may be the consumption of poorly washed vegetables and fruits. Staphylococci enter the body with food (when visiting, for example, a public canteen, where food is prepared by a person who has a wound on the skin of the hand). Infection also occurs through direct contact of a child with a sick adult or baby.
Video: Ways of infection of children with staphylococcal infection. Features of treatment
Symptoms of staphylococcal infection in children
Staphylococcal infection occurs in 2 forms - early and late. The early form is a disease, the manifestations of which occur within a few hours after the onset of the pathological development of staphylococci in the body. The late form appears only after a few days (from 3 to 5).
Typical signs of a staphylococcal infection in a child are:
- the appearance of pustular rashes and abscesses on the skin;
- stomatitis (inflammation of the oral mucosa), conjunctivitis;
- cramps and colic in the abdomen, increased flatulence, diarrhea.
At the same time, the child’s temperature rises to 38°-38.5°. He feels nauseous and vomits. The baby is capricious and weak. Symptoms of the disease in each specific case depend on the location of the pathogen, the age of the patient, its development, the presence of previous diseases, and the state of immunity.
In which organs is Staphylococcus aureus found most often?
Most often, staphylococcal infection affects the gastrointestinal tract, ENT organs, skin, and eyes. Accordingly, intestinal dysbiosis, inflammatory throat diseases, conjunctivitis, and skin rashes are observed.
Much less often (in children with low weight, who have serious congenital or acquired diseases, who have undergone surgery), the lungs, brain, heart, joints and circulatory system are affected.
Symptoms of intestinal infection
Possible damage to the rectum (colitis) or the entire intestine (enterocolitis). In children, the effect of staphylococcus on the intestinal mucosa leads to spasmodic pain in the abdomen and a feeling of heaviness in the stomach. There is an enlargement of the liver and spleen. Nausea and vomiting appear. Possible increase in temperature.

The stool is liquid, green, with admixtures of mucus, pus and blood. Often there is a false urge to have a bowel movement. There are signs of dehydration: dry mouth, crying without tears, infrequent urination, headache, circles under the eyes, wrinkling of the skin.
Signs of damage to the throat and oral mucosa
Symptoms of sore throat occur: sore throat when swallowing, redness and inflammation of the tonsils. Rashes appear on the gums (stomatitis), as well as signs of intoxication of the whole body (high fever, nausea, dizziness, headache, convulsions).
Damage to the nasal mucosa
A purulent runny nose occurs. The nose is stuffy due to swelling of the mucous membrane. Inflammation quickly spreads to the maxillary sinuses. The child breathes through his mouth. His body temperature rises and other signs of intoxication appear.
Symptoms of skin infection
In children, staphylococcal infections often develop in the skin. The bacterium does not die under the influence of salt, which contains human sweat, which protects the skin from many other microorganisms. Penetrating into the pores, the microbe begins to destroy sebum cells, which are produced by the sebaceous glands located at the base of the hairs. In this case, the hair follicles become inflamed.
Purulent pustules appear on the affected areas of the skin. Their accidental damage leads to the rapid spread of infection to neighboring areas. In the absence of timely treatment, deep abscesses (boils) appear, which merge with each other, forming carbuncles that are difficult to heal. Possible formation of boils and barley.
Signs of development of staphylococcal infection in infants
In an infant, Staphylococcus aureus often affects the respiratory organs, which leads to staphylococcal pneumonia. A newborn may become ill already in the hospital. Moreover, the infection develops rapidly. Intoxication of the body leads to the appearance of symptoms such as respiratory failure, dry cough, severe sweating, and elevated body temperature.

Possible inflammation of the umbilical wound. Swelling on the face, a rash on the skin, and purulent discharge from the nose appear. The infection spreads quickly, affecting the intestines. Abdominal bloating, increased passage of gas, and diarrhea occur. The baby refuses to breastfeed, spits up often, and quickly loses weight. If treatment is ineffective, death may occur.
Diagnostics
If a child shows signs of developing a staphylococcal infection, it is necessary to consult a doctor to do tests of blood, stool, urine, nasal discharge, oral swab, and skin swabs.
The blood is examined to detect antibodies to staphylococci in the serum. PCR analysis makes it possible to clarify the type of infection based on the characteristic composition of DNA molecules. A general blood test allows you to determine the presence of an inflammatory process, determine the level of hemoglobin and other characteristic changes in indicators.
If staphylococcal bacteria are found in the stool of an infant, and their number exceeds the norm, an analysis of the mother's milk is done to clarify the cause of the baby's infection. If the test result is positive, the child is transferred to artificial nutrition.
In order to choose the most effective antibiotic, bacteriological culture of swabs from the nose and throat is done to determine the sensitivity of microbes to certain drugs.
If necessary, an endoscopic examination of the intestine is performed to detect the extent of damage to the mucosa.

Treatment principle
According to most pediatricians, the reason for starting treatment should be a significant excess of the norm in the content of staphylococci in children in the blood, feces, as well as the presence of obvious symptoms of the disease. For example, the famous children's doctor E. Komarovsky in his articles and lectures emphasizes that it is necessary to start treatment with antibiotics only when the baby has green mucus, blood, pus in the stool, as well as the formation of ulcers on the head or blood poisoning. In other cases, the main goal of treatment is to strengthen the immune system.
If the skin is damaged, it is treated with bactericidal agents (brilliant is especially effective), as well as ointments with antibacterial and cell-regenerating drugs are applied. They are selected strictly taking into account the age of the child, and are used only as prescribed by a doctor. Vishnevsky ointment is often used for treatment.
You can relieve inflammation and swelling of the skin and eliminate purulent rashes using decoctions of string, celandine, calendula, chamomile, and oak bark. You can make lotions or arrange medicinal baths.
For intestinal diseases, as well as for severe complications in other organs, antibiotics are prescribed. Moreover, the use of an incorrectly chosen drug leads to the development of particularly strong resistance in bacteria to the action of antibiotics. In this case, there will be even more problems with treatment.
A sore throat and nasal mucosa are treated with an antiseptic solution of miramistin, and rinsed with solutions of iodinol or silver nitrate.
For sepsis, a blood transfusion or plasma infusion is performed. In some cases, it is impossible to do without surgical operations, such as removing tonsils or removing ulcers on the skin.
To strengthen the immune system, children are given vitamins and immunomodulators.

Prevention
In order to prevent children from becoming infected with staphylococci and the development of infection, it is necessary, first of all, to follow the rules of hygienic care for the baby, to accustom him to cleanliness and neatness. You should not buy food for a small child from random street vendors, or give him sausage, smoked meats, or canned food.
It is necessary to take care of strengthening the baby’s immunity: hardening the body, physical development, good nutrition. In order to prevent the development of staphylococcal infection in newborns, mandatory examination of pregnant women is carried out.
The content of the article
The concept " staphylococcal infection“combines any diseases caused by staphylococcus, that is, it is based on the unity of etiology.
Staphylococcus capable of infecting almost all tissues and organs of the human body. Clinical manifestations of staphylococcal infection are very diverse and are named mainly by the localization of the process: rhinitis, tonsillitis, nasopharyngitis, lymphadenitis, otitis media, laryngitis, arthritis, meningitis, etc.
In this regard, diseases of staphylococcal etiology are considered separately. However, these diseases have common patterns: a single etiological origin, close epidemiological and pathogenetic connections, common morphological changes and clinical manifestations. They can occur in the form of independent diseases and are very common as additional layers, as a secondary infection, as a mixed infection in various pathological processes, especially in young children. Therefore, it is necessary to consider the group of staphylococcal infections as a whole with a description of general provisions, general patterns that are directly related to infectious diseases, to the differential diagnosis of infections, to epidemiology.
The combination of different staphylococcal processes into the group of staphylococcal infections as a whole turned out to be progressive and fruitful in terms of their study. Thus, the concept of “staphylococcal infection” includes any staphylococcal diseases and the so-called carriage of pathogenic staphylococcus, which in epidemic terms represents the same danger as the disease.
It is necessary to keep in mind the difficulty of distinguishing carriage from the mildest, subclinical inapparent forms of staphylococcal processes, the frequency of which is high.
Etiology of staphylococcal infection in children
The causative agents of diseases combined into the group of staphylococcal infections are staphylococci, belonging to the group of micrococci (mycrococcus pyogenes), they received their name from their characteristic arrangement in a microscopic specimen in the form of clusters; from the Greek words “staphylion” - bunch and “kokkos” - grain.Staphylococci have a spherical shape, stain well with Gram and all aniline dyes, are immobile, do not form spores, are aerobes and facultative anaerobes. Staphylococci grow well on ordinary nutrient media with a slightly alkaline reaction at a temperature of 35 - 37 ° C. In the broth, they first form a uniform turbidity, and then a loose flaky sediment, which later turns into a viscous mass. On solid media (agar), staphylococci grow in the form of large, opaque colonies.
Of the solid media, the most commonly used are yolk-salt (Chistovich's medium), blood and meat-extract agar.
It is customary to distinguish between pathogenic strains and saprophytes. In the past, only Staphylococcus aureus was considered pathogenic; later it turned out that among the white and yellow ones there could also be highly pathogenic and toxigenic cultures. Pathogenic staphylococci are distinguished by their ability to secrete toxins and enzymes that disrupt the vital activity of the cells of the macroorganism and destroy its tissues.
Pathogenic staphylococci secrete a soluble exotoxin; it consists of many components that can be in different proportions:
- lethal toxin causes death when injected into a rabbit;
- necrotic toxin or dermonecrotoxin, when administered intradermally, causes skin necrosis;
- leukocidin causes the death of leukocytes;
- staphylolysin destroys red blood cells (when growing on blood agar, it provides a hemolysis zone around the colonies).
This is the main toxin secreted by all toxigenic strains of staphylococci. In addition to it, there are toxins secreted only by some staphylococci: enterotoxin And erythrogenic toxin.
Enterotoxin little studied, isolated from crops that intensively seeded food products, mainly milk and cream products.
Erythrogenic toxin secreted by a few hemolyzing staphylococci, the nature of its action is close to Dick's streptococcal toxin. When administered to volunteers, it causes the same symptoms of intoxication and scarlet fever syndrome as Dick's toxin (spot rash). The intradermal reaction with staphylococcal erythrogenic toxin is the same as the Dick reaction with streptococcal toxin.
In addition to exotoxin, pathogenic staphylococci secrete enzymes that promote the rapid spread of the microbe in the body - enzymes of “defense and aggression” (G. N. Chistovich):
- coagulase - promotes plasma coagulation;
- hyaluronidase - dissolves collagen layers and promotes the spread of the microbe (spread factor, hyaluronidase);
- proteinases - dissolve proteins;
- lipase;
- phosphatase - dissolves fats and lipoids;
- lecithinase - dissolves lecitoverillin;
- staphyloagglutinin - agglutinates red blood cells;
- antiphagin - inhibits the action of the phage;
- penicillinase - inactivates penicillin.
Pathogenic and toxigenic properties do not always coincide. In the pathological process, different enzymes and toxins usually have a complex effect; individual clinical forms can develop with the predominant influence of certain mechanisms of staphylococcal aggression.
In the external environment, staphylococci tolerate drying, high and low temperatures, direct sunlight, are resistant to many chemicals, and are durable in dust, on things, linen and toys. When their living conditions change, both in vitro and in a living organism, staphylococci can change morphologically and culturally, they can change serological types, from virulent they become saprophytes and from saprophytes they can turn into highly pathogenic and toxigenic. The adaptability of staphylococci to drugs and, in particular, to antibiotics is very high. In hospitals, multidrug-resistant strains are often isolated from staff and from long-term hospitalized patients. They are called hospital strains.
Epidemiology of staphylococcal infection in children
The source of staphylococcal infection is humans- a patient with any form of staphylococcal infection or a carrier. The most dangerous patients are those with lesions respiratory tract and pharynx, as they can secrete staphylococci and spread them around over a considerable distance with droplets of infected sputum and mucus, especially when coughing. Patients with copious purulent discharge from wounds are also dangerous. Pus saturates the bandages and, when dried on them, turns into dry dust, which spreads in the air over long distances.The epidemic danger is often more pronounced in mild, mild forms of infection; protective measures are rarely taken in them; they often support the chain of infection and can cause a fatal infection in the recipient.
The duration of infectiousness of patients in most cases is long even after recovery. Staphylococci can persist for months and even years. With intensive therapy with active antibiotics, sanitation of the microbial focus can occur quite quickly, but often a carriage or chronic infection remains with the presence of a dormant focus.
In carriers, the main place of localization of staphylococcus is the nasal cavity and skin. As sources of infection, carriers play an extremely important role, since they usually remain in groups, where they disperse the infection. The isolation of pathogenic staphylococcus from the feces of children, especially infants, and its inoculation from the blood should be treated with great caution. Usually it does not mean carriage, but the presence of some staphylococcal inflammatory focus in the body.
In newborns, children of the first year of life, children weakened by any other diseases, blood culture and non-pathogenic strains (if the blood is taken correctly) usually also indicates the presence of a staphylococcal process. This is also evidenced by repeated seeding of the microbe from the blood and massive contamination.
Distribution routes Staphylococcal infections are different, but mainly they are airborne and dust.
The contact and household route of transmission is also very important; infection can occur through objects, hands, dressings, dishes, linen, etc. There is also a food route of transmission through contaminated food products when they are eaten.
Finally, an injection method of infection is also possible, while staphylococcus enters the body during medical procedures, due to insufficient treatment of instruments, defects in injection technique, and the introduction of substandard medicines. In this regard, glucose solutions, which are a good nutrient medium for staphylococci, are especially dangerous; they can easily become infected if preparation or storage is defective.
Pets can also be a source of infection, but their epidemiological significance is negligible. In the external environment, independent reservoirs of pathogenic staphylococci apparently do not exist.
Susceptibility to staphylococcal infection is different and depends on age and condition. It is highest in newborns, infants, the elderly, and also in patients.
Patients with acute viral diseases (influenza, measles, viral hepatitis), blood diseases, diabetes, postoperative patients and patients with extensive skin lesions (eczema, burns) are especially susceptible to staphylococci. Susceptibility to staphylococci increases with long-term use of corticosteroids and cytostatics.
Morbidity staphylococcal infections is very high, but exact data does not exist. Staphylococcal infections often occur sporadically, but there can be family, group diseases and significant epidemic outbreaks, which most often occur in hospitals - in orphanages, maternity hospitals, etc.; Outbreaks of staphylococcal foodborne illnesses may occur.
Mortality from staphylococcal infection remains at significant levels, and as mortality from other diseases decreases, the proportion of staphylococcal infection among the causes of death is high.
According to hospitals different countries and different cities, staphylococcal infection as the direct cause of death is in first place.
Staphylococcal infections have always been dangerous as nosocomial diseases; they can take on the character of disasters, sometimes affecting even well-maintained institutions.
The intrahospital spread of staphylococci is facilitated by insufficient identification and elimination of the sources of the disease (patients with mild staphylococcal processes and carriers, including staff), overcrowding, violation of the sanitary regime, insufficient sterilization of instruments, dressings, etc.
G. N. Chistovich, using phagotyping, identified the spread of staphylococcus among newborns, where he established the following chains of infections:
Among newborns, infections with pathogenic staphylococcus through mother's milk are common, especially if mothers have mastitis.
Staphylococcal infections in hospitals are usually an exogenous infection.
Pathogenesis and pathological anatomy of staphylococcal infection in children
Staphylococci are introduced into the body through the skin, mucous membranes of the pharynx, oral cavity, respiratory tract, and genitals; through the conjunctiva. The pathological process unfolds as a result of the interaction of the pathogen and the child’s body. Thus, there are, as it were, two sides of the process unfolding in the external environment.Exposure to pathogen. The pathogenic activity of staphylococci corresponds to the processes of their life activity: nutrition, reproduction, growth, development. In the process of this vital activity, staphylococci secrete enzymes and toxins that destroy tissue, absorbing, assimilating these tissue breakdown products. In the body, due to the effects of toxins, enzymes, and tissue destruction by staphylococci, pathological changes appear that affect the dysfunction of tissues and organs. In addition, compensatory and protective reactions occur in the body.
This entire two-way process is complex and very dynamic: the child’s body changes, staphylococci undergo changes, the external environment in which the pathological process develops changes.
To deploy the process, in addition to infection, a number of additional conditions: pathogenic activity of staphylococci, their virulence; sufficient dose of infection (sufficient number of staphylococci); violation of tissue integrity and reduction of specific protection and nonspecific resistance of the child’s body.
The normal epithelium of the skin and mucous membranes with their secretion serves as a good anatomical defense against the introduction of staphylococcus into the body, and staphylococcal infection occurs as a result of a violation of this barrier. That is why staphylococcal infection is widespread among patients with acute respiratory viral infection. The pattern of development of staphylococcal infection following an acute viral infection has been pathomorphologically confirmed, which is established by corresponding changes in the epithelium, virus release, immunological data, or the presence of viral inclusions in the affected tissues (O. I. Bazan, V. A. Tsinzerling, etc.). Damage to the epithelial cover during acute respiratory viral infection creates a wound surface in the respiratory tract, which is one of the main reasons for the frequent subsequent development of tracheitis, laryngitis, bronchitis, pneumonia, and bronchiolitis.
The importance of specific protection and nonspecific resistance is confirmed by the age distribution of staphylococcal diseases and their occurrence in the presence of aggravating factors.
Most often, newborns and young children weakened by previous illnesses become ill. Staphylococcal infections are common in children with blood diseases due to damage to the function of the reticuloendothelial system and other disorders; for eating disorders, during treatment with corticosteroids that suppress immunological reactions; in newborns who have suffered birth injuries. In such cases, low pathogenic staphylococci may also be the etiological factor.
Different localization of the pathological process in combination with different conditions of infection determine the extremely wide variety of clinical manifestations of staphylococcal infection - from the mildest lesions to the most severe fatal diseases. Virulent strains of staphylococcus in high concentrations in healthy older children can lead to the emergence of mild, subclinical forms. Along with this, in a weakened child at an early age, strains of low virulence can cause severe forms of infection.
At the site of introduction of staphylococci in the body, a local inflammatory focus appears, most often in organs that have a connection with the external environment (skin, nasopharynx, tonsils, respiratory tract, intestines). In the affected area, accumulation of staphylococci, circulatory disorders, edema, tissue infiltration, hemorrhages, stasis, blood clots in capillaries and small vessels, fibrin formation, a tendency to suppuration, and tissue necrosis are observed. There are several main forms of inflammation: catarrhal, purulent, necrotic, fibrinous.
In catarrhal forms, infiltration of the mucous membrane, submucosal layer, plethora, stasis, serous exudate mixed with mucus and leukocytes, cellular exudate, phagocytosis are observed at the site of inflammation; the same changes in surrounding tissues.
For purulent forms in places where staphylococci accumulate, tissue breakdown, purulent, catarrhal-purulent, serous-hemorrhagic exudate, phagocytosis processes, and effusion around the lesion are noted.
For necrotic forms inflammation is characterized by predominantly necrotic, serous-hemorrhagic tissue breakdown in the lesion.
Necrotic changes in the respiratory tract (laryngotracheitis) are also manifested by necrosis of the mucous and submucosal membranes with the formation of ulcers covered with white dull deposits. With necrotizing pneumonia, disintegration of bronchial tissue, lung tissue, and connective tissue septa occurs. Multiple foci of destruction lead to the formation of thin-walled cavities, the sizes of which are labile due to the involvement of new areas of lung tissue in the process.
Fibrinous inflammation in severe processes can acquire a dominant character, on the basis of which the fibrinous (diphtheritic) form is isolated. Fibrinous tonsillitis has been described with the formation of thick gray-white films on the affected surface of the tonsils. There is a diphtheritic form of laryngotracheitis with the formation of fibrinous films in the larynx and especially in the trachea; fibrinous pleurisy is common. Necrotic, fibrinous-necrotic inflammation can occur in the intestines and other organs.
The distinction between different forms of inflammation based on predominantly pronounced changes that acquire paramount importance is rather arbitrary. And with the catarrhal form there may be superficial necrosis, suppuration, and fibrin loss. However, with necrotic, purulent, fibrinous forms, these changes are especially significant.
One form of inflammation can transform into another. The catarrhal form is essentially the initial form of inflammation; in many patients at this stage the process ends, is localized and resolves with the help of phagocytosis and other protective reactions. It is very important for the clinician to prevent its progression in a timely manner.
Special attention. deserve pneumonia, which, as a rule, is present in all children who die from staphylococcal infection. Staphylococci penetrate the respiratory tract through the bronchogenic route. At the site of microbial penetration, foci of inflammation develop, often purulent, purulent-necrotic in nature, with tissue disintegration, which contributes to the formation of a cavity. Purulent foci - abscesses can be multiple. The pleura is also often involved in the process with the development of fibrinous-purulent pleurisy and empyema. A subpleural abscess may rupture into the pleural cavity, followed by pyopneumothorax. In some cases, bullous emphysema is determined. Air cavities are considered pathognomonic for staphylococcal pneumonia.
Among staphylococcal pneumonias, a group of pneumonias without destruction and tissue disintegration stands out; in the clinic they sharply predominate. Among pneumonias without destruction of lung tissue, processes are observed in the very initial stage of development - focal or confluent bronchopneumonia without necrotic lesions and perifocal toxic changes.
The body's protective reactions at the site of inflammation, in regional lymph nodes, are carried out by a local tissue barrier, phagocytosis of staphylococci by leukocytes. Many patients do not have a tendency to progressively spread the staphylococcal lesion; by phagocytosis reactions it is fixed in the form of a local process. The changes are eliminated by resorption of the exudate.
Along with this, if treated incorrectly, or if exposed to any additional factors that reduce resistance, especially in infancy, generalization of infection from a local focus may occur. Intracanalicular spread of infection causes inflammation in the paranasal cavities, middle ear, and respiratory tract. Staphylococcus can penetrate the blood, spread hematogenously, cause osteomyelitis, arthritis, endocarditis, etc. Transfer of infection from a local focus can occur lymphogenously - this is usually the way lymphadenitis and peritonitis occur. Generalization of infection occurs in different ways in the same patient. For example, at the same time it spreads from the nasopharynx intracanalicularly into the accessory cavities, lymphogenously into the lymph nodes and hematogenously into any joints.
As a result of the generalization of the infection, sepsis and septicopyemia can develop, especially often occurring in early infancy, and among them in children in the first 3 months of life, and in newborns.
With staphylococcal diseases, bacteremia is very often detected, most typical for infants. Staphylococci do not multiply in the blood, so bacteremia indicates the presence of a staphylococcal inflammatory focus in the body.
Microbes, entering the blood, partially die, and are partially removed from the body through the respiratory tract, urinary system, and gastrointestinal tract.
In the local inflammatory focus, staphylococci produce toxins, which, when absorbed, have a general toxic effect on the body. The reticuloendothelial system is involved in the process, which is illustrated by changes in the spleen (reproduction of reticular cells) and liver (dystrophic changes). Changes occur in the lungs (increased blood supply, focal atelectasis, emphysema, etc.), dystrophic changes in the myocardium (protein degeneration, sometimes degenerative obesity of muscle fibers). In the kidneys, changes in the interstitial tissue, leukocyte infiltrates, congestion of the medulla, and interstitial serous nephritis may appear.
Microbial breakdown products have a sensitizing effect. Allergic changes are promoted by repeated staphylococcal infections and constant carriage of staphylococcus. It is possible that staphylococci may participate in the development of allergies with the occurrence of nephritis and rheumatism.
In the pathogenesis of staphylococcal infection, the following syndromes are distinguished: infectious septic, toxic and allergic. Their combination determines the entire infectious process as a whole.
For infectious septic syndrome characterized by the presence of inflammatory foci, always present in any form of staphylococcal infection. The degree of their severity ranges from minimal minor to profound violations.
Toxic syndrome is unique. A huge number of local mild staphylococcal processes occur without noticeable signs of intoxication, in other cases they can manifest as low-grade fever, a mild disturbance of general well-being and appetite; with a long course can lead to anemia, to changes characteristic of hemolytic disease; in infants they may cause insufficient weight gain.
In severe inflammatory lesions, the toxic syndrome with its usual manifestations (fever, often vomiting, cardiovascular disorders) is already quite pronounced; intoxication can be violent with a quick legal outcome.
Allergic syndrome occurs due to the sensitizing effect of microbial decay products, it is MMHIILHCICM using skin tests; its clinical manifestations have been almost completely studied.
IN last years Chronic forms of staphylococcal infection have begun to attract much attention. Their occurrence is associated mainly with improper, insufficient treatment for acute forms and with the adaptive ability of staphylococci, as a result of which they can acquire the same properties as human proteins. Due to this, they lose almost ion irritation, the production of antibodies decreases and the process becomes sluggish, protracted or chronic course.
Immunity has not been studied enough. Antibacterial immunity is absent or unstable, and does not protect against diseases during repeated infections with staphylococcus, even of the same phagotype. Antitoxic immunity is developed mainly after suffering from a severe toxic form of the disease. The presence of antitoxic antibodies (antihemolysins and antileukocidins) in the blood, even in high titers, does not prevent the development of subsequent purulent processes. The phagocytic reaction plays a major role in staphylococcal immunity.
Clinic of staphylococcal infection in children
Staphylococcal infection is characterized by exceptional clinical diversity, very difficult to classify. Generalized and predominantly localized forms can be distinguished, although this division is very arbitrary.To generalized forms include sepsis, septicopyemia. Predominantly localized forms are distinguished by the presence of lesions in any specific area of the body. With localized forms, metastatic foci are also often observed, as, for example, with tonsillitis, lymphadenitis, otitis media. However, in contrast to generalized forms, these lesions retain a local character and therefore can be classified as localized with the proviso “predominantly”. Localized forms can be severe, such as osteomyelitis, but are classified in this category due to the specific local location of the staphylococcal process. Sometimes it is very difficult to draw the line between generalized and localized forms.
Localized forms are usually diagnosed by the location of the inflammatory process, depending on the damage to a particular organ: rhinitis, tonsillitis, lymphadenitis, otitis media, pneumonia, etc.
It is impossible to identify characteristic forms due to the absence of clinical signs typical of staphylococcal diseases, with the exception of the formation of air cavities in pneumonia. We can only talk about pronounced clinical forms, subclinical and inapparent forms.
Staphylococcal process can be primary or secondary. Primary is the one from which the disease begins; secondary is the process that develops in the presence of an existing focus. There are mild, moderate and severe forms of staphylococcal infection. According to the course, acute, protracted and chronic forms are distinguished. Below is a diagram of the localization of the staphylococcal inflammatory process and associated clinical manifestations.
The most common localization of staphylococcal diseases are the skin and subcutaneous tissue, pharynx, nose, nasopharynx and respiratory tract. Diseases of the digestive tract (enterocolitis), bone lesions, etc. are often encountered.
The incubation period lasts from several hours to 3-4 days. The onset of the disease is acute. In the local inflammatory focus, catarrhal changes occur (hyperemia, usually localized swelling due to swelling of the underlying tissues); mild pain. With more severe lesions, a purulent inflammatory process is formed, and finally, fibrinous-necrotic changes may occur in the local focus. Hyperemia becomes intense, infiltration of the affected tissues is pronounced, and deposits appear in the form of dirty, loose, grayish deposits located on the ulcerated surface. When fibrin is deposited, plaque forms in the form of dense films on infiltrated hyperemic tissues. The process is often mixed purulent-necrotic, fibrinous-necrotic in nature.
Regional lymph nodes enlarge in different ways, sometimes reaching sizes chicken egg; their contours are predominantly blurred due to the infiltration of surrounding tissue, but they can also be sharply contoured. When suppuration occurs, pain appears, the skin over the glands turns red, and fluctuation begins to be detected in the depths.
In many patients with catarrhal changes in the local focus, the disease passes without symptoms of intoxication. With more significant local inflammation, intoxication appears without any features specific to staphylococcus. The temperature during staphylococcal infection can be normal, low-grade, or reach 39-40 ° C or more, mainly in accordance with the severity of inflammation.
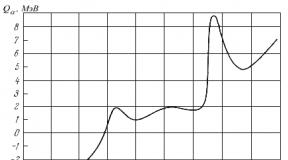
A blood test reveals leukocytosis, neutrophilia with a shift to the left, and increased ESR. The degree of changes and intoxication corresponds to the severity of the disease and the severity of inflammation. In severe processes, leukocytosis sometimes reaches 20 - 30-109 per liter, neutrophil shift can be down to myelocytes, ESR rises to 30-40 mm per hour or more. The development of hypochromic anemia is typical, especially in young children.
Towards light forms include diseases that occur without disturbance or with a slight disturbance in general well-being, at normal or subfebrile temperature, without any special functional disorders in the body. Among staphylococcal diseases, the most common are these mild forms in the form of rhinitis, nasopharyngitis, catarrhal tonsillitis, minor diarrhea, skin lesions with mild inflammatory changes and a shift in the leukocyte formula of the blood. Such forms are difficult to diagnose, yet they pose a danger for a number of reasons. Accompanying another disease, especially acute respiratory viral infection, a mild, harmless disease can cause a severe process. Without treatment, such a disease can continue for a long time (weeks, months), developing into a chronic process. Patients suffering from mild forms can become a source of infection for others. Mild forms can be observed at any age, in weakened children in the form of sluggish skin lesions, rhinitis, tonsillitis; in infancy - in the form of minor bowel irregularities.
Subclinical forms Staphylococcal infections occur without visible local inflammatory foci. They can only manifest as low-grade fever, moderate leukocytosis, sometimes neutrophilia, especially an increase in ESR. Infants with such forms may only have a flat weight curve, impaired appetite, sometimes regurgitation, and anemia. The presence of such forms is confirmed by bacteriological data, immunological reactions, and in children the agglutination reaction with staphylococcus becomes positive. In infants, staphylococcus is often cultured from the blood.
Inapparate forms They do not manifest themselves clinically and are detected only on the basis of immunological changes.
Severe forms Staphylococcal infections are characterized by high fever, anxiety, impaired consciousness, there may be vomiting, increasing pallor, cyanosis. The pulse quickens, may be thread-like, and blood pressure drops. In severe forms, various rashes often appear, and hemorrhages are not uncommon. Severe forms with intoxication usually develop with a pronounced exudative component, with suppuration, necrotic, fibrinous changes in the local focus. These include laryngotracheitis, bronchiolitis, abscess pneumonia, pleurisy, meningitis, sepsis, etc. Severe septic changes develop slowly, since the appearance of sufficiently pronounced anatomical changes in the form of a significant inflammatory purulent, purulent-necrotic, fibrinous focus or even multiple foci requires a certain time, usually several days. In a number of cases, an acute onset is noted, but it is only apparent; as a rule, it is preceded by subtle, visible, and non-diagnosable changes. I believe that with a rapid increase in intoxication, toxic forms arise in the form of acute gastroenterocolitis and scarlet-like syndrome, which can develop with relatively moderate local changes, but toxic damage to the central nervous system.
Currently, with the availability of effective medicinal products severe forms with septic syndrome in many patients can be attributed to advanced cases that appear as a result of underestimation of initial changes, incorrect assessment of the dynamics of changes, and improper treatment.
Moderate forms include cases with moderately severe intoxication. The body temperature is increased to 38-39° C, the general condition is disturbed, but not sharply. Heart changes are limited to moderate tachycardia, muffled heart sounds. Headache and decreased appetite are noted. Local local processes in moderate forms are predominantly purulent, necrotic, fibrinous in nature, but are more limited in distribution and depth of damage. The dysfunction of the affected tissues and organs is also less pronounced. Moderate forms often include tonsillitis, phlegmon, pneumonia, enterocolitis, etc.
The course of staphylococcal diseases can be acute when the process ends in the first weeks or 1-2 months, protracted when recovery is delayed for several months, and chronic when the process lasts not only months, but also years. During the course of the disease, exacerbations, repeated temperature waves, temperature “candles,” and low-grade fever are often observed. The tendency for a long course is high, especially in weakened children, in children in the first months of life. A protracted and chronic course can take on both mild forms in the form of rhinitis, tonsillitis, otitis, and severe forms, in particular osteomyelitis. Exacerbations may occur, especially during acute viral infections, when a staphylococcal infection can manifest itself as the rapid development of pneumonia and sepsis.
Bacteremia is characteristic, which appears in any form (subclinical, inapparent), but still mainly in severe or chronic forms. In infants and weakened children, bacteremia can persist not only for weeks, but for months and even years. It is usually supported by sluggish dermatitis, rhinitis, tonsillitis, sinusitis, otitis, process in the biliary and urinary tracts, etc.
Selected clinical forms of staphylococcal infection in children
Various lesions of the skin and subcutaneous tissue are most common in children, especially young children, and newborns. Staphylococci can cause infection in diaper rash, cause paronychia, panaritium, phlegmon, impetigo, etc. Any of these processes can occur in isolation or in combination with others, occur during sepsis or be the primary septic focus.Nasal lesion
When the nose, pharynx, and nasopharynx are affected, rhinitis, pharyngitis, nasopharyngitis, and tonsillitis occur, which contribute to the formation of peritonsillar abscesses, otitis, lymphadenitis, and sinusitis. Damage to the respiratory and digestive organs is often associated with damage to the nose and pharynx.Respiratory lesions
Respiratory system lesions are very diverse. Depending on the location of the infection, laryngitis, tracheitis, bronchitis, bronchiolitis, pneumonia, pleurisy appear, and they are often combined.Clinical manifestations of damage to the respiratory system are primarily a cough, a disturbance in general well-being, mainly with temperature reactions. Laryngitis and laryngotracheitis are among the common, often severe forms of staphylococcal infection. Due to the predominant combination with acute respiratory viral infection, cough often appears against the background of other catarrhal phenomena (runny nose, sneezing).
The disease develops mainly within 1-2 days, often accompanied by laryngeal stenosis (croup). Stenosing laryngitis and laryngotracheitis are among the severe forms of staphylococcal infection due to severe functional disorders. There are no patterns in the occurrence and development of croup of staphylococcal nature. For some, the disease begins immediately with symptoms of stenosis, while for others, difficulty breathing develops later against the background of previous benign laryngitis. As with diphtheria croup, there are 4 degrees of stenosis. However, stenosis in croup of staphylococcal etiology does not develop strictly in a certain sequence. It can occur suddenly at the onset of the disease and be of a pronounced nature; it can also develop at a later date.
Laryngitis, laryngotracheitis often occurs with pneumonia; with croup it is observed in almost all cases.
Pneumonia Staphylococcal infections can be primary or secondary, occur either as an isolated process, or are one of the foci of infection localized in the body. In recent years, staphylococcus has been the main etiological factor in the occurrence of pneumonia in young children.
Staphylococcal pneumonia occurs mainly in the form of ordinary small-focal pneumonia, often with catarrh of the upper respiratory tract. The disease can end quickly, can drag on and proceed rather sluggishly, or become more pronounced, accompanied by hyperthermia (39-40 ° C and above). Resolution of pneumonia usually occurs gradually, with low-grade fever lasting for a long time. Destructive forms of pneumonia are the most severe. Sometimes they develop quite quickly, and in the coming days abscesses and pyopneumothorax form. In other cases, the disease develops more gradually against the background of prolonged catarrh of the upper respiratory tract. Against this background, the condition worsens sharply, and a clinical picture of acute pneumonia develops. The “explosion” can also occur against the background of previous mild localized pneumonia, seemingly during the recovery period. Subsequently, the development of these initially different processes occurs in the same way. In this case, intoxication, respiratory, and heart failure are usually pronounced. Severe staphylococcal pneumonia is characterized by radiological data: in the lungs with destructive pneumonia, small foci of darkening are first detected, then they reach large sizes. After 1-2 days, areas of clearing appear (round, but irregular in shape) or cavities with clearly visible oval contours, in some cases with a horizontal level.
Damage to bones and joints
When bones and joints are affected, osteomyelitis and arthritis occur, which are described in detail in surgical manuals. Osteomyelitis in newborns, young children and infants develops mainly as a result of generalization of purulent infection in the body and is very difficult to diagnose.This is a serious disease that requires early treatment to prevent severe forms. Bone damage at this age is often multiple, the most severe is osteomyelitis of the pelvic bones and spine. At older ages, the processes are predominantly isolated and proceed more favorably.
Damage to the central nervous system
Damage to the central nervous system of staphylococcal nature can be in the form of meningitis and brain abscess, which are characterized by the most severe course.Staphylococcal meningitis is usually a secondary process that occurs as a result of generalization of infection. The primary focus can be localized in the ears, paranasal sinuses, skull bones, etc.
The disease occurs with severe intoxication and rapidly developing meningeal symptoms (stiff neck, Kernig-Brudzinsky sign). As a result of intoxication, patients often develop a rash on the body, which is generally characteristic of severe staphylococcal diseases.
In infants, the disease is most severe, usually in a general septic condition. During a spinal puncture, cerebrospinal fluid flows out under increased pressure and is cloudy and greenish-gray in color. The protein content is increased, neutrophilic cytosis is pronounced.
During the course of the disease, exacerbations of the process and repeated temperature waves are often observed. Inflammatory purulent changes from the meninges pass to the substance of the brain, causing brain abscesses. They can also be present in osteomyelitis of the skull bones, like metastatic foci in septicopyemia. These are rare, but extremely severe processes that are difficult to diagnose. When they are located in the silent zone, focal symptoms may be absent; the main diagnostic method is radiography.
Urinary tract lesions
In case of defeat urinary tract cystitis, pyelitis, pyelonephritis, focal nephritis occur. These diseases are often observed in severe forms of staphylococcal infection and, above all, in sepsis. In mild forms, they are facilitated by the duration and recurrence of diseases; chronic processes are very unfavorable in this regard.Damages of the cardiovascular system
Defeats of cardio-vascular system can be in the form of endocarditis, pericarditis, phlebitis. Endocarditis is very difficult to diagnose and is often discovered only posthumously. They are also observed nowadays in long-term diseases, mainly in young children and infants. Pericarditis has been extremely rare in recent decades. Phlebitis is a particular form of staphylococcal infection that occurs as a complication of skin and subcutaneous inflammatory processes. Phlebitis can worsen the course of the main process and cause the emergence of new lesions. This is one of the ways to develop sepsis with multiple purulent foci, especially in the joints and kidneys.Sepsis
Sepsis is predominantly a problem for young children. The entrance gate, as in other forms, can be the skin if its integrity is violated.mucous membranes of the respiratory tract, gastrointestinal tract, umbilical wound in newborns. Sepsis can develop latently, slowly and unnoticeably, but often rapidly, with lightning speed. Secondary septic foci can be in any part of the body, but most often they are localized in the lungs and ears. In young children, diarrhea occurs in most cases; Damage to the bones and heart (septic endocarditis) is common. Intoxication is manifested by the usual changes; rashes of different types often appear: small-spotted, pinpointed, urticarial, hemorrhagic. The current course of sepsis with proper treatment is generally favorable, but complete recovery is still slow.
During bacteriological examination, a pronounced contamination of patients with staphylococcus is determined; bacteremia lasts a long time.
Mixed infection
Staphylococcal infection is detected in almost all infectious diseases. Isolation of pathogenic staphylococcus from patients upon admission to hospital and frequent subsequent infection were detected. The most common staphylococcal processes are rhinitis, nasopharyngitis, acute tonsillitis, and exacerbations of chronic tonsillitis. Manifestations of staphylococcal infection, in addition, are temperature reactions, especially low-grade fever, blood changes without visible local processes, pneumonia, including in the form of destructive forms, and sepsis. Staphylococcal cholangitis and cholecystitis are observed. Staphylococcal infection reaches its maximum frequency in acute respiratory viral infections, especially in infants.The diagnosis of mixed infection should be established as soon as possible early dates for timely treatment, while the formation of severe forms can be sharply reduced. Severe forms are predominantly advanced forms of infection due to delayed diagnosis and improper treatment of the disease. Signs of staphylococcal infection in other diseases (as a mixed infection) are the same as in monoinfection.
Diagnosis, differential diagnosis of staphylococcal infection in children
The main symptom of staphylococcal infection is inflammation with a tendency to suppuration with the formation of thick pus with a greenish tint, and a tendency to fibrinous deposits. It is very important to take into account the absence of any pronounced patterns during staphylococcal infection, both at the beginning and during the course of the disease. This is an uncertain nature of the temperature reaction with temperature returns, temperature “candles”, low-grade fever, etc. The most constant changes in the blood (leukocytosis, neutrophilia, increased ESR). It is most often necessary to differentiate from acute viral and microbial, mainly streptococcal infections, which is extremely difficult. Streptococci cause rhinitis, tonsillitis, lymphadenitis, otitis, pneumonia, etc. Streptococcal and staphylococcal infections have similarities in pathogenesis and pathomorphological changes. With streptococcal, as with staphylococcal, infections, the pathogenesis includes infectious, toxic, and allergic syndromes. Both infections are characterized by the appearance of purulent, purulent-necrotic inflammation; a form with a pronounced effect of erythrogenic toxin may occur.Of the clinical differential signs, one can note only a slightly greater severity of hyperemia and other inflammatory changes in streptococcal lesions, which is clearly identified in tonsillitis. In staphylococcal processes, hyperemia often has a cyanotic tint, and a predominant lesion of the nasopharynx in the form of enlargement of the posterior cervical lymph nodes is characteristic.
Streptococci do not cause boils, carbuncles, or damage to the intestinal tract in the form of diarrhea. Streptococcal lesions of the pharynx, ears, and lymph nodes are more acute, more dynamic, and characterized by a faster development of the process, but all these differences are not sharp enough and require a lot of experience to identify. Streptococcal processes are quickly resolved after the first injections of penicillin, even in moderate dosages, while at the same time, penicillin acts on staphylococcal lesions in large dosages, and even then not always.
In case of staphylococcal infection with scarlet fever syndrome, the basis for differential diagnosis is not so much individual symptoms as the sequence of their development, the combination of individual symptoms. In the presence of fibrinous inflammation in the pharynx, it is differentiated. occurs with a localized form of diphtheria of the pharynx. Diphtheria is characterized by low severity of inflammatory changes, the presence of dense fibrinous films of a grayish-white color without suppuration, protruding above the surface of the tonsils, and moderate pain. The temperature in such forms of diphtheria rises moderately and decreases over the next 2 to 3 days.
Changes characteristic of staphylococcal tonsillitis can be observed in infectious mononucleosis.
This depends mainly on the layering of the staphylococcal process in mononucleosis. In these cases, there are other signs characteristic of mononucleosis: polyadenitis, an increase in the size of the liver and spleen, a fairly persistent temperature reaction, and the slow disappearance of these changes. The final diagnosis of mononucleosis is made on the basis of hematological changes. The layer of staphylococcal infection is determined as a result of bacteriological examination.
The main difference between staphylococcal lesions and acute laryngitis, laryngotracheitis, and croup of diphtheria etiology is the absence of any patterns in the development of the process. The disease can develop both acutely and gradually. Hoarseness of voice, barking cough and difficulty breathing may immediately appear. Stenosis can immediately reach II and III degrees; grows rapidly, interspersed with periods of calm. The voice becomes hoarse, but aphonia usually does not occur. In addition, laryngotracheitis of staphylococcal etiology develops, as a rule, against the background of a septic condition, with high fever and pneumonia. The pharynx is hyperemic, swollen, the mucous membranes are juicy. In contrast, with diphtheria the process develops naturally, one stage gradually, over 3-4 days, passes into another. With isolated diphtheria damage to the larynx, there may not be any special changes in the pharynx, but with a combined form (diphtheria of the larynx and pharynx), tonsillitis is determined with dense fibrinous, filmy deposits characteristic of diphtheria.
Laboratory methods for diagnosing staphylococcal infection
The diagnosis of staphylococcal infection is established primarily on the basis of clinical changes, but in mild, subclinical forms laboratory data are especially necessary. However, even with obvious forms, at present, without laboratory confirmation, a clinical diagnosis, with rare exceptions, is not considered competent.Laboratory examination includes bacteriological and serological methods. The bacteriological method is of paramount importance. Both methods are simple and easily accessible to ordinary laboratories.
Bacteriological research. Depending on the location of the inflammatory focus, mucus from the nose, pharynx, oral cavity, and larynx is examined, the skin, wounds, closed purulent foci, etc. are examined. In case of damage to the gastrointestinal tract, the material being examined can be vomit, rinsing water, and feces. Blood cultures should be performed as widely as possible, since bacteremia is common in staphylococcal infections.
A full examination should be carried out on sectional material from the lesions, and in addition, regardless of the location of the lesion, the tissue of the tonsils, lungs, liver, spleen, small and large intestines, stomach, their contents, tissue of the mesentery, and lymph nodes.
Intravital examination should be carried out as early as possible from the onset of the disease, preferably before the use of etiotropic treatment, which helps reduce seeding. In addition, the study must be repeated.
Sowing staphylococcus has not only diagnostic value, but allows us to judge the progress of the pathological process. Prolonged massive contamination reflects the severity of the pathological process and requires further persistent treatment, preferably until complete bacteriological cleansing. If massive contamination persists, the process may worsen. Next, it is necessary to examine children with an already established diagnosis of a disease of non-staphylococcal nature (measles, dysentery, coli infection, viral hepatitis, etc.), who have an atypical course of the disease, low-grade fever, blood changes in the form of leukocytosis, increased ESR, anemia.
Mucus from the pharynx, nose, and larynx is taken on an empty stomach before medical procedures, which can also affect seeding. During the day, it can be taken no earlier than 2 hours after eating, drinking, or taking medications.
The discharge from the wound is examined before treatment.
Blood for inoculation is taken with strict adherence to the rules of asepsis and antiseptics in an amount of 3-5 ml, inoculation is carried out in 50 ml of sugar broth. The inoculated broth is kept in a thermostat for 5 days: daily the broth is inoculated onto blood agar.
In bile, each portion is examined separately (A, B and C).
The milk of a nursing mother is collected in a sterile container after preliminary thorough treatment of the mammary gland with a sterile breast pump and after preliminary pumping. For the study, 3-5 ml of milk is taken separately from each mammary gland, centrifuged and inoculated on blood agar and Chistovich's medium.
When seeding from the test materials, the pathogenicity of staphylococcus is determined.
For serological testing, an agglutination reaction similar to the Widal reaction is used.
The most conclusive is the examination of the patient over time: at the beginning of the disease and subsequently with a break of 10-14 days. During these periods, many patients experience an increase in titer in dilutions of agglutinating serum. A one-time examination of the patient is also possible; diagnostic titer of the agglutination reaction is 1:100 or higher. The agglutination reaction has not only diagnostic value, but to a certain extent reflects the course of the disease. The positive reaction does not last long, as titers improve, it can quickly decrease, and later, during recovery, it turns negative. It is also valuable that the agglutination reaction gives good results in weakened children, young children and newborns.
In recent years, determination of alpha antitoxin in blood serum has been used. The reaction uses the patient’s blood serum and alpha toxin, and red blood cells are added as an indicator. The presence of antitoxic properties of blood serum is judged by the inhibition of hemolysis in vitro. The diagnostic value of increasing antistaphylolysin titer and allergic reactions is being studied.
In conclusion, it must be pointed out that the diagnosis of staphylococcal infection is based on a careful assessment of clinical changes. Despite the absence of pathognomonic symptoms, the clinical manifestations of staphylococcal infection are sufficiently expressive to establish or suspect its presence not only in mild cases, but often even in subclinical forms of the disease. The diagnosis is made definitively based on a set of clinical changes and laboratory test results.
Features of staphylococcal infection in modern conditions
Staphylococcal infection currently occupies one of the first places among microbial infections in its distribution. There is constant talk about a significant increase in the number of diseases of staphylococcal etiology, but there is no exact data, because they were not registered before and currently the records are imperfect. Along with this, it has been reliably established that the proportion of staphylococcal infection among severe forms of microbial processes and among the causes of death has sharply increased; in this regard, it came out on top, and this is especially noticeable in relation to pneumonia. Until the 40s of our century, pneumococci had the leading etiological significance in pneumonia, and the frequency of streptococcal processes was significant. After the introduction of sulfonamide drugs effective against pneumococcus into practice, streptococcal lung lesions, often of an abscess nature, took first place. Further changes occurred mainly from the early 50s, after the introduction of penicillin. It has a rapid reversing effect on both pneumococcal and streptococcal processes, and they have become very rare.Staphylococci, due to their ability to quickly adapt, quickly acquired resistance to penicillin and took first place among severe purulent inflammatory lesions. The situation with staphylococcal infection began to improve since the 60s with the introduction of broad-spectrum antibiotics, the use of large doses of penicillin, the development of pathogenetic treatment methods, and the preparation of specific drugs. All this taken together has made it possible to significantly reduce the mortality rate of staphylococcal infections, however, staphylococcal processes in all their diversity occupy one of the leading places in the pathology of children.
Treatment of staphylococcal infections in children
IN complex treatment Staphylococcal infection is based on the impact on the pathogen, i.e. on eliminating the cause without which the disease would be impossible at all. With timely, effective elimination of the pathogen, other treatment tasks (impact on the body, on the inflammatory focus) often become unnecessary. It is also the main thing in preventing the development of severe forms.
The influence on the causative agent of the disease is carried out by etiotropic means.
Treatment of acute mild forms (catarrhal tonsillitis, rhinitis in older people) is not required. Antibacterial therapy should be used in cases where the process becomes protracted, blood changes persist, low-grade fever appears, a tendency to increase local changes with suspicion of pneumonia, and a tendency to generalize inflammatory processes. All patients with severe and moderate forms, any forms of staphylococcal infection that occur in children with any other diseases are subject to treatment.
Staphylococcal infection worsens the course of the underlying disease, which in turn affects the course of the staphylococcal process. In a hospital setting, in the presence of a mixed staphylococcal infection, antibacterial therapy is also necessary because the patient is a source of infection for others.
Currently, there are many antibiotics that act on staphylococcus; the choice of one or another drug for each patient is carried out individually. For full treatment it is necessary to follow a number of rules set out in the general part.
For mild and moderate forms in older children, one antibiotic is sufficient; in more severe cases, two are used simultaneously; for particularly severe forms, three antibiotics are used, taking into account their synergistic effect. For severe, generalized forms of staphylococcal infection, it is necessary to use new antibiotics, broad-spectrum antibiotics.
In infants, in patients with multiple lesions, especially with mixed infections, treatment with antibiotics in separate courses with a change in the drug often has to be carried out for several weeks until the pathological changes are completely eliminated, low-grade fever and blood changes are eliminated.
From the large arsenal of antibiotics, penicillin retains its value, which is indicated only in increased and large doses. The daily dose (from 200,000 to 500,000 units/kg or more) is administered intramuscularly after 3-4 hours. Penicillin can be used in combination with monomycin, kanamycin and other antibiotics.
Semi-synthetic penicillin preparations are very effective in cases where penicillin has no effect in the presence of pathogens resistant to it.
Penicillin can be used for mild to moderate forms of the disease, leaving broad-spectrum antibiotics as a reserve for severe forms, for those cases in which penicillin has no effect. The use of tetracyclines and chloramphenicol is currently limited, and is contraindicated in children in the first months of life due to their greater toxicity.
To prevent the development of dysbiosis during antibiotic treatment, it is necessary to simultaneously prescribe nystatin, levorin, B vitamins, and vitamin C.
Phages have a direct effect on staphylococcus; they are able to lyse pathogenic strains; they are used mainly for lesions of the outer integument (staphyloderma, suppuration of wounds). Used locally in the form of lotions.
The effect on the patient’s body is achieved by both specific and pathogenetic means. Specific agents are aimed at strengthening specific immune defenses. They are used in combination with antibiotics. Hyperimmune antistaphylococcal gamma globulin, which is used for severe, generalized forms of staphylococcal infection, especially for the treatment of young children, has received wide recognition. It is administered intramuscularly at 5-6 AE/kg per day daily or every other day - 5-7 times. In especially severe cases, the daily dose is increased to 20 AE/kg. Hyperimmune antistaphylococcal plasma is administered intravenously daily or every 1-3 days, 5-8 ml/kg, 3-5 times in total. The blood of immunized donors is used mainly through direct transfusion from the donor to a child in the amount of 4-8 ml/kg several times with an interval of 3-4 days.
Native staphylococcal toxoid is used to increase the production of staphylococcal antitoxin in the body in prolonged, sluggish forms. There are two schemes for using toxoid, which is injected subcutaneously under the shoulder blade. According to the first scheme, 7 injections are given with an interval of 2 - 3 days (0.1-0.2 - 0.3-0.4-0.6-0.8-1.0), a total of 3.4 ml. According to the second scheme, 5 injections are given with an interval of the first day (0.1-0.5-1.0-1.0-1.0), a total of 3.6 ml.
In order to increase the production of antibodies (mainly in dermatological practice), staphylococcal antifagin is used.
Pathogenetic agents
Pathogenetic agents are prescribed according to indications. For severe, toxic forms of staphylococcal infection, conventional detoxification therapy is used. The use of corticosteroids is recommended. Cortisone, hydrocortisone, prednisolone are prescribed as a short course (5-7 days) with a gradual reduction in dose as the patient's condition improves. In especially severe cases, they begin with intramuscular or even intravenous administration of drugs. When administering corticosteroids, potassium salts are indicated.For the purpose of detoxification, intravenous drip infusions of 5% glucose solution with saline solutions, plasma solutions, and plasma substitutes are used. To this are added diuretics:
Lasix, Novurit, Mannitol. Large doses are administered simultaneously ascorbic acid, cocarboxylase.
For disorders of the cardiovascular system, corglycone and strophanthin are used. Desensitizing drugs (diphenhydramine orally or intramuscularly) are also used.
For hyperthermia, usually observed in severe neurotoxicosis, antipyretic drugs (amidopyrine with analgin), drip, intrarectal administration of chilled glucose solutions, cold on the head and large vessels are indicated.
For encephalitic syndrome and meningeal symptoms, a spinal puncture is necessary; for convulsions, magnesium sulfate, chloral hydrate in enemas, other drugs with sedative properties (sodium hydroxybutyrate), and neuroplegics (aminazine, pipolfen) are prescribed. For vasomotor complex syndrome, vasoconstrictors, warming, glucose, and plasma-substituting solutions are used. In cases of exicosis, which is observed mainly in intestinal forms of staphylococcal infection, it is necessary to administer copious amounts of fluid intravenously - from several hours to several days, depending on the patient’s condition.
In severe forms of staphylococcal infection, acute respiratory failure may develop. In these cases, it is necessary to suction the mucus from the pharynx and larynx with an electric suction device. The viscous thick exudate is liquefied by soda inhalations and proteolytic enzymes (chymotrypsin). To ensure sufficient oxygen supply, patients are placed in DKP-1 oxygen tents, where humidified oxygen is supplied.
If pneumothorax, pyopneumothorax, or empyema occurs, urgent surgical intervention is necessary.
For laryngotracheitis, laryngoscopy is indicated to remove crusts and mucus from the tracheal lumen. They resort to soda inhalations and mustard plasters. In cases of degree II-III stenosis, prolonged intubation through the nose using a polyethylene catheter is used. In the absence of effect, prolonged oxygen deficiency, a tracheostomy is performed.
Symptomatic therapy
Symptomatic therapy involves influencing individual symptoms of the disease. In modern conditions, it is usually carried out taking into account the essence of the pathological process and the mechanism of action medicine, therefore very close to pathogenetic therapy.Physiotherapeutic methods
Physiotherapeutic methods are an integral part of treatment. These are compresses, heating pads, ice, cold, mustard plasters, mustard wraps, baths, paraffin applications, etc. Ultraviolet rays, diathermy, UHF, etc. are widely used.Surgical methods of treatment
Surgical treatment methods are used mainly for purulent complications.Acute mild, moderate forms usually respond well to timely and sufficient antibacterial treatment. The temperature quickly drops to normal, the general condition improves;
changes in the source of inflammation are eliminated more slowly, and blood normalization is often delayed. In addition to antibiotics and vitamins, other medications are used according to indications.
In severe forms of staphylococcal infection, in addition to the specific therapy listed above and means to combat severe toxicosis, repeated blood transfusions (5-7) after 4-5 days have a good effect. The best option is direct blood transfusion. Symptomatic agents are used according to indications.
In patients with prolonged; In recent years, biological drugs have been proposed for treatment of chronic forms: colibacterin, lactobacterin, bifidumbacterin, bificol. They are used to combat dysbiosis in order to normalize the intestinal flora, especially in intestinal forms of staphylococcal infection. Biological drugs are prescribed according to special regimens outlined in the prospectuses.
Mothers of infants who have any staphylococcal diseases must be treated with antibiotics. Otherwise, the child will almost inevitably become infected. Preventive measures must be strictly followed. If the pharynx and respiratory tract are affected, feeding and caring for the child is carried out only with masks; in case of skin lesions, communication with the child is limited, etc. In case of staphylococcal lesions of the mammary gland in a nursing mother, it is necessary to use local agents and antibiotics during treatment. Breast milk should be expressed and given only boiled or pasteurized.
Staphylococcus aureus- a bacterium that produces a strong toxin and has an adverse effect on the human body. This bacterium lives in the body in small quantities without causing harm, but if the immune system is weakened, staphylococcus begins to actively multiply and leads to the development of purulent-inflammatory processes. Staphylococcus aureus is especially dangerous for infants, since babies have an undeveloped immune system and are not able to withstand the aggressive effects of the microorganism.
Against the background of infection with this bacterium, they can develop a variety of pathologies, including the most severe ones, such as and. And since Staphylococcus aureus is predominantly a nosocomial infection, infants become infected with it immediately after birth - from the mother, contaminated objects or personnel.
Causes of staphylococcal infection
Staphylococcus aureus appears in newborns in several cases. Firstly, if the baby becomes infected from a sick mother or a mother carrying the bacteria. In this case, infection can occur in three ways:
- when a woman has contact with a child;
- when feeding through breast milk;
- infection can occur directly during the passage of the child through the mother’s birth canal.
Secondly, Staphylococcus aureus can appear in a newborn if personal hygiene rules are not followed in a medical facility or at home. For example, if the mother does not wash the baby often enough, washes his hands, etc., because the child constantly puts something in his mouth, but is everywhere around us, and can easily get on the body and hands.
Also, staphylococcus often appears in newborns due to infection from maternity hospital medical staff. This happens in cases where health workers were not promptly identified with this pathogen or they do not thoroughly clean their hands before performing procedures for caring for the baby in a maternity hospital, which is why staphylococcus from environment and falls on the newborn.
By airborne droplets, Staphylococcus aureus can also enter the body of a newborn, but in this case it causes pathologies such as staphylococcal etiology. Sometimes newborns become infected with this bacterium through the umbilical wound, again due to insufficient hygiene by the maternity hospital staff or the mother herself.
Staphylococcus is detected in a certain amount in the body of every newborn, but not everyone provokes the development of dangerous pathologies. Most often they develop in children who have reduced immunity. Predisposing factors to the development of the disease may be:
- prematurity;
- pathological course of pregnancy and delivery;
- malnutrition of the newborn.
It can also develop in children who have gone home in cases where they are often sick and their immune defenses are compromised. Parents may also encounter this pathology in a child suffering from.
Symptoms
The signs that Staphylococcus aureus has entered the baby’s body are different, because everything depends on the immune defense, the aggressiveness of the microbe and its location. Most often, Staphylococcus aureus affects the oral cavity and respiratory tract, as well as the digestive tract - this is due to the main routes of infection into the infant’s body.
If the bacteria has settled in the nose, symptoms such as:
- rhinitis with slight discharge;
- loss of appetite;
- weight loss.
The general condition of the newborn is usually not disturbed, the temperature does not rise.
In cases where the microbe enters the oral cavity, staphylococcal, or, develops.
The signs of such a lesion are as follows:
- purulent-necrotic plaque on the palate, tonsils, tongue;
- hyperemia of the pharynx, which does not have a clear localization;
- elevated temperature.
Usually, when staphylococcus is detected in the throat of a newborn, he has a very sore throat, but the child cannot complain of pain, so parents can guess that this symptom is present by the fact that the baby refuses food and cries (the crying intensifies when swallowing).
Despite the fact that the routes of infection with Staphylococcus aureus can be different, the most popular route of infection in newborns is food, so staphylococcus is very often found in the feces of infants, which normally should not be there. If staphylococcus is detected in the feces of a newborn, it means that there is a possibility that he will develop or.
Signs that a microorganism has entered the child’s gastrointestinal tract are as follows:
- vomiting that is non-stop;
- pale skin;
- diarrhea up to 6 times a day;
- skin rashes - from boils to neonatal pemphigus.
Also, symptoms of disorders in the gastrointestinal tract due to a staphylococcal infection may be as follows - abdominal pain, dizziness, weakness. But a small child cannot tell about these symptoms, so their presence is evidenced by his behavior - tearfulness, moodiness, refusal to eat, etc. Older children may already complain about certain signs, based on which the doctor can assume the presence in the body of staphylococcal infection.
A very serious complication of staphylococcus in a newborn can be when the microbe spreads through the blood throughout the body. Sepsis often causes death, which is why it is so important to begin treatment of the pathology in a timely manner.
Diagnosis and treatment
Staphylococcus aureus is found in stool or nasopharyngeal swabs of infants. Also, when making a diagnosis, the doctor takes into account the complaints of the child’s parents and his general well-being. Treatment must be carried out in a hospital setting, and the baby and his mother must be placed in separate boxes, since this infection is contagious to other hospital patients.
Typically, treatment includes antibacterial drugs, which are prescribed in combination (several at once) to prevent the bacteria from developing resistance to them. It is advisable, before starting treatment, to determine the sensitivity of the pathogen to antibiotics - then it will be more effective. Treatment also involves the use of antistaphylococcal drugs and detoxification therapy. At the same time, treatment should be aimed at increasing the child’s immunity, for which the baby is prescribed vitamin complexes.
If Staphylococcus aureus is found in the intestines of a small patient, probiotic preparations, for example, Bifidumbacterin, should be included in the treatment.
Unfortunately, staphylococcus is difficult to treat, so treatment can be lengthy, and its results are assessed by repeated bacterial culture or taking stool for analysis.
Is everything in the article correct from a medical point of view?
Answer only if you have proven medical knowledge
Diseases with similar symptoms:
Pneumonia (officially pneumonia) is an inflammatory process in one or both respiratory organs, which is usually of an infectious nature and is caused by various viruses, bacteria and fungi. In ancient times, this disease was considered one of the most dangerous, and although modern treatments make it possible to get rid of the infection quickly and without consequences, the disease has not lost its relevance. According to official data, in our country every year about a million people suffer from pneumonia in one form or another.
Even in the maternity hospital, mothers hear about a threatening disease that creates health problems in newborns. The type of bacteria that causes it got its name due to the spherical or oblong shape of the cells arranged in the form of clusters. From Greek kokkas is translated as “grain”, staphylos - “bunch”. Are these bacteria really that dangerous?
general information
The name of the bacteria coincides with the designation of an infectious disease that is dangerous to the health of children. It does not threaten children with a sufficient level of immunity. However, as soon as the protective forces weaken, the infection begins to actively develop.
Staphylococcus bacteria can provoke inflammation of the respiratory tract. Staphylococcal pneumonia can develop even before discharge from the hospital. Severe intoxication of the microorganism occurs.
In combination with pneumonia, infection causes circulatory and respiratory system problems. Staphylococcal enterocolitis can be fatal.
How staphylococcus is transmitted in children, how the symptoms of the infection manifest themselves and how it can be cured, we will discuss below.
Causes
The only cause of staphylococcal infection is violation of local immunity. Carriers of harmful bacteria are both sick and completely healthy people.
And bacteria become harmful only when the child’s body’s defense mechanisms have begun to fail or are not yet strong enough.
The development of infection can be triggered by:
- Premature birth of an underweight child.
- Failure to comply with the rules of care for newborns.
- Pathologies during the gestation period, when infection occurs at the stage of fetal development.
- Infection during breastfeeding from a mother infected with staphylococcus.
Types of disease
Not all members of the staphylococcal family pose a threat to children's health. Some of them coexist quite well in body fluids and tissues. Three types of staphylococcus are considered pathogenic:
- Saprophytic. The least dangerous for humans, and even more so for children. It strikes more often genitourinary system. With proper treatment, you can get rid of the microbe in a few days.
- Epidermal (epidermic) staphylococcus in children. It is found on all areas of the skin and mucous membrane of the nose, eyes, and oral cavity. It is not dangerous for a healthy child and is even considered normal if the child feels well. At risk are babies who were born prematurely, weakened babies, and patients after surgery.
- Golden. Poses the greatest danger. This is the most insidious of microorganisms. It can be found on the surface of the skin, in the mouth, and in feces. If the child is healthy, then the body copes with these bacteria on its own.
The cunning of a microorganism is associated with its ability to adapt to different conditions.
Golden staphylococcus is not afraid of low and high temperatures. It can withstand even +80 degrees. It adapts to the effects of most antiseptics and antibiotics, so treatment with the latter is often ineffective. Resistant to hydrogen peroxide, ethyl alcohol, sodium chloride.
About the signs, symptoms and treatment of Staphylococcus aureus in children, watch the video of Dr. Komarovsky:
\There are two forms of the disease:
- Early symptoms appear a few hours after the bacteria enters the child’s body.
- Late. It makes itself known only after 3-5 days.
Symptoms and general signs

Staphylococcal infection is indicated by:
If the disease is not diagnosed in time, the infection can affect internal organs.
Manifestations of defeat
The organs affected are different depending on the method of infection penetration into the body, most often the risk zone is the throat, nose and intestines. Different forms of staphylococcus in a child have their own specific symptoms:
- in the intestines: diarrhea, constipation, heaviness and abdominal pain, bloating, impurities of pus, mucus in the stool;
- in the nose: swelling and difficulty breathing, purulent discharge, intoxication of the body;
- in the mouth and throat: swelling and redness of the tonsils, sore throat, rashes on the surface of the oral mucosa, manifestations of intoxication.
How to recognize a disease in a child

Parents cannot diagnose the disease. Their task is to monitor the child’s condition and reactions. The intensity and nature of the infection is influenced by:
- Age. Newborns suffer from staphylococcus infections more often, and the consequences are much more serious.
- The way bacteria enter the body. If staphylococcus is carried with dust particles, this can lead to respiratory tract infection. If the bacteria enters the body with food, the intestines and throat will be affected.
- When the baby is often sick, and the parents know that he is weakened the immune system, it makes sense to worry when suspicious symptoms appear.
You cannot self-medicate. It is necessary to consult a doctor who will examine the child and give a referral for tests.
Diagnostic measures
Results only laboratory research will be able to confirm that the symptoms are caused by a staphylococcal infection. If the amount of staphylococcus in the analysis does not exceed the norm, and there are no symptoms of infection, then there is nothing to worry about.
To determine the norm, a number of studies are carried out:

If the pathology process has gone too far, for example, with colitis caused by staphylococcus, an endoscopic examination may be necessary to assess the condition of the colon. For staphylococcus that has infected the throat and reached the larynx, laryngoscopy is performed.
Did you know that mononucleosis can occur completely unnoticed? Read about infectious mononucleosis in children.
In the next article, we will introduce you to eye exercises for myopia for children. Be sure to check it out!
And you will learn how enuresis in children is treated at home.
Treatment methods and regimens
When the diagnosis is confirmed, all tests are done, doctors prescribe a course of treatment. How to treat staphylococcus in a child? Therapy may include:
In rare cases in case of severe infection, blood transfusion is used and plasma. Surgery cannot be ruled out.
When treating a child, it is important to follow the rules of hygiene:
- The child's skin should be dry and clean, nails should be trimmed, and underwear should be fresh.
- All household items, dishes, and clothing used by the child must be disinfected.
It is not always necessary to treat staphylococcus in a child - watch the video on this topic:
Prevention
The unformed and weakened organism of infants is most susceptible to infection by staphylococcus, which is why its symptoms appear. It is easier for older children to fight off bacteria, but only if they are healthy. Preventive measures to strengthen defense mechanisms:
- Proper nutrition, excluding fast foods, unhealthy fats, and sweets.
- Active lifestyle - swimming, athletics, gymnastics, regular walks in the fresh air.
- Compliance with the rules of personal hygiene - regular water treatments, proper oral care, the habit of washing your hands after a walk or visiting public places.
- Protecting the baby from stress: problems in the family, nervousness of adults.
These measures will help avoid attacks by harmful bacteria and unwanted consequences.
Staphylococcal infection is dangerous for both newborns and older children, Staphylococcus aureus is especially dangerous. Symptoms of the disease manifest themselves differently depending on the method of penetration of dangerous bacteria. But a healthy child’s body with a strong immune system is not at risk of infection.
To prevent staphylococcal infection in infants, expectant mothers need to take care of their health in advance and promptly inform doctors about changes in the baby’s behavior. Older children need to be taught the rules of hygiene, a balanced diet and an active lifestyle.
In contact with
Read also...
- Will I get married? Fortune telling online. Fortune telling for a new acquaintance. Fortune telling with playing cards Fortune telling by a friend
- Morozov Nikolay Aleksandrovich Nikolay Morozov Narodnaya Volya
- You can cook French fries in the microwave How to make your own French fries in the microwave
- Crispy pickled cucumbers in jars