Infectious diseases: list, modes of transmission, symptoms, treatment and prevention. Blood infection. Causative agents of blood infections. Disease prevention How infection spreads through blood
AIDS
AIDS stands for "acquired immunodeficiency syndrome." Term "syndrome" means the presence of a whole complex of manifestations, the cause of which is unknown, "acquired" - This means that it is not congenital, but appeared after birth, "immunodeficiencycit" - This is a condition in which the body's defenses, or immunity, are destroyed.
Although the causative agent of the disease, the virus HIV, has already been identified, the term AIDS continues to be used. HIV destroys the immune system, making the body susceptible to various infections and diseases. These infections, like tumor diseases, are secondary in nature, that is, they develop as a result of
shared favorable conditions. The virus is not directly related to them. Diseases arise due to the destruction of the immune system, which loses the ability to fight microorganisms.
HIV is not dangerous through normal household contacts. It is found in large quantities in sperm and is transmitted only during sexual intercourse, especially anal: it is extremely rare in homosexual women. It is also transmitted through contaminated vaginal secretions, through injection needles, through contaminated blood transfusions, and finally through contaminated milk from a mother infected with the virus.
Initially, the disease is asymptomatic. Signs may take many months or even years to appear. HIV works as follows.
- Infection: The virus enters the body and infects cells. The person feels fine and is not yet sick with AIDS.
- Disease: the first phase resembles infectious mononucleosis. Some patients do not go through this stage; they begin the next phase directly.
- Antibody production: Antibodies are produced to fight the HIV virus, usually a month or two after infection.
- Occurrence of SPI syndrome Yes: this syndrome is a serious condition indicating that the immune system is significantly compromised.
- SP Detection Yes: AIDS is usually discovered when a rare infection or tumor makes itself known. From this moment on, the patient has an average of 1 year of life.
- Death: successive manifestations of a serious illness occur until one of them becomes the cause of death.
Signs of AIDS:
Feeling constantly tired - for no apparent reason.
Fever, chills, or night sweats that appear for no apparent reason and last for several weeks.
Weight loss for no apparent reason - more than 5 kg or 10% of the initial weight within 1-2 months.
Enlarged lymph nodes in the neck, armpits, or groin, without an obvious cause and lasting more than 2 months.
Pink, red or brown, flat or raised spots or papules. They can appear on the nasal mucosa, in the mouth, on the eyelids or in the anus.
White or other unusual spots in the mouth.
Frequent diarrhea.
Constant dry cough, especially with suffocation.
Most of these symptoms can also be observed with other, less serious diseases. They do not necessarily mean AIDS. However, if you have had questionable sex or been in situations where you could be infected, do not wait for symptoms to appear. Antibodies that are produced during AIDS are formed in the blood only a month after infection, so immediate testing is not effective. Most clinics and hospitals conduct an examination two months after treatment. If the result is negative, the test should be repeated after six months - perhaps antibodies began to be produced later.
If the result is positive, you can contact a help group, where they can provide psychological assistance better than in institutions. Don't try to fight the disease alone.
AIDS is a terrible disease that takes many young lives. There is currently no vaccine against the virus and treatment is ineffective. Zidovudine (AZT), for example, slows the progression of the disease. Intensive research is being conducted into ways to prevent, early diagnose and treat AIDS. ‘So far, the only true method of prevention for homosexual men is contact with only one partner or complete abstinence. The data obtained indicate that the number of casual relationships between homosexuals has indeed decreased significantly. Some young men consider AIDS a disease of the elderly. They believe that by choosing a partner under 25 years of age and engaging exclusively in oral sex, they are protected from infection. Nevertheless, two cases of AIDS infection in this way are definitely known. Everything suggests that young men will also have to limit themselves to one sexual partner.
A serious problem is that among people with heterosexual orientation the number of casual relationships does not decrease. In 1989, 749 women and 386 men developed AIDS as a result of
heterosexual contacts. The only reliable means of protection against the threat of AIDS is complete monogamy in sex. Condoms protect against infection with the virus, but do not provide a 100% guarantee.
Hospitals now control blood and blood products very strictly. Blood tests and transfusions are believed to be harmless. But, for example, drug addicts who inject themselves sometimes use contaminated needles when injecting, so in this risk group the number of infected people increases significantly. The disease also began to spread among students and secondary school students.
Until December 31, 1988, there were 89,764 cases of SPI House reported in the United States, of which 90% occurred in men. The average age of patients is 37 years. Among the cases, about 68% of gay or bisexual men did not use intravenous drugs, 17% had received intravenous injections, 2% had undergone blood transfusions in the past, and 1% were people with hemophilia or other blood diseases.
Average age women infected with AIDS - 35.7 years. Some women become infected from a sick partner after several intercourses, others do not become infected even after several hundred. Surveys of women whose husbands suffered from hemophilia and were carriers of HIV showed that only 15% of women were infected; 22 women whose partners did not use condoms became infected; In 14 women whose partners used condoms, the virus was not detected.
In December 1988, there were 1,346 children with AIDS in America; 82% are under 5 years of age, of which 40% are less than a year old. By the end of December 1988, 56% of all AIDS patients and 85% of those diagnosed with HIV before 1986 had died. AIDS deaths accounted for 9% of total deaths in those aged 25–34 years and 7% of total deaths in those aged 34–44 years.
When the AIDS epidemic was first declared in the United States in 1981, almost all cases were white men, gay men or people who had received blood transfusions. In 1989, more than 11% of new diseases occurred in women, and 23% were intravenous drug users.
In the 90s, due to the growth of drug addiction in the United States, the virus began to spread among heterosexuals and women. It affected entire families, especially among the black poor.
According to the Center for Combating infectious diseases, more than 2 million American citizens are infected with the AIDS virus. These terrifying numbers speak for themselves.
In July 1990, information was received from Great Britain that a vaccine against HIV had been found. However, it will still be a long time before clinical studies confirm the effectiveness and safety of the vaccine.
Hepatitis
Hepatitis (liver inflammation) A and B is caused by a virus. The virus is found in feces and is transmitted through contaminated food and water. It can sometimes be transmitted through sexual contact, rarely through contaminated blood transfusions. Maintain personal hygiene. Avoidanal and oral sex.
Symptoms of viral hepatitis A occur 15-40 days after infection. The temperature rises, nausea appears, headache, weakness, chills and loss of appetite. After a week, the skin, nails and whites of the eyes acquire a yellow tint, which lasts for about 3 weeks; the urine is dark, the stool is almost colorless. Some people do not have these signs. The immune system begins to produce antibodies against the virus, which, however, remains in the blood and can infect others. These people are carriers diseases.
The symptoms of viral hepatitis B are similar to those of hepatitis A. However, they become apparent very suddenly, 1-6 months after infection, and the disease is more severe. In case of severe liver damage, 5-20% of patients die. Recovery occurs very slowly, and in 20% of cases, liver disease becomes chronic and leads to cirrhosis. New drugs are now being developed, which gives some hope.
Viral hepatitis A is transmitted through blood and its products, as well as through semen, saliva and feces during sexual intercourse. Now it is classified as a sexually transmitted disease. Drug addicts who use dirty needles also become infected with it. The prevalence of hepatitis is increasing, presumably as a result of the growing number of intravenous drug users. Homosexuals, people with many sexual partners, tourists and drug addicts are especially at risk.
There are approximately 300,000 cases of viral hepatitis in the United States each year, mostly in young people. About 25% have celiac disease
severe, more than 100,000 require hospitalization. Every year, 350-400 people die from viral hepatitis A. Carriers of virus B are susceptible to liver cancer. It is believed that 4,000 people die annually from cirrhosis caused by hepatitis B, and over 1,000 die from liver cancer associated with viral inflammation.
After any questionable sexual contact or if any symptoms appear, get tested immediately. At the first signs of illness, consult a doctor. When caring for patients with viral hepatitis, carefully observe the rules of personal hygiene. All things that the sick person has touched - soap, towels, shaving accessories, etc. - can be contaminated and should not be used by healthy people.
Gamma globulin injections provide reliable protection for 5 years. The second dose of the drug is administered a month later, and the third - 6 months after the first. Three doses are required for reliable protection against the disease. Homosexuals need to have regular blood tests to determine their level of immunity or the presence of the virus.
Vaginitis (inflammation of the vagina)
The vagina is not sterile - it contains many harmless microorganisms, just like a man's urethra. Fungi or bacteria have a favorable environment for development here. Under certain conditions, these fungi, Trichomonas (protozoa), can develop quite strongly and cause inflammation. Its symptoms are itching, burning, swelling, burning during urination and discharge with an unpleasant odor.
Inflammation of the vagina (vaginitis) is not transmitted sexually. Antibiotics or dietary changes can disrupt the vaginal flora and cause yeast infections. This disease is considered “purely female.” But Trichomonas or Gardnerella can cause inflammation of the urethra in a man, and they can also become infected with fungi. The head of the penis hurts and itches, and after a few days tiny ulcers appear.
Failure to maintain genital hygiene promotes reproductionnium of microorganisms. Less commonly, bacteria enter the urethra or prostate gland. The man is unaware of the infection because there are no signs of the disease. He is an asymptomatic carrier of the disease. If the partner is being treated, he is also required to undergo treatment.
Instructions
AIDS is an acquired immunodeficiency syndrome that develops as a result of exposure to immune system human immunodeficiency virus (HIV). Cells of the immune system, central nervous system, red and white blood are damaged. Syphilis is a chronic systemic disease caused by bacteria of the species Treponema pallidum (treponema pallidum). It is characterized by damage to the skin, mucous membranes, internal organs, bones, and nervous system with a sequential change in the stages of the disease. Viral hepatitis is an inflammation of liver tissue caused by viruses related to different types and differing in biochemical characteristics: hepatitis A virus, hepatitis B virus, hepatitis C virus. Brucellosis is an acute or chronic disease characterized by damage to the nervous system, bones and joints. Leprosy is a chronic disease affecting the skin, peripheral nervous system, eyes, hands and feet.
Echinococcosis is a disease caused by Echinococcus. Accompanied by damage to the liver, lungs, brain, muscles, kidneys. Toxoplasmosis is a disease caused by Toxoplasma. Symptoms: fever, enlarged liver, spleen, headache, vomiting. Filariasis is a helminthic disease affecting the subcutaneous tissue, serous membranes, eyes, and lymph nodes. Leishmaniasis is a disease that occurs with ulcers of the skin and mucous membranes, with severe damage to internal organs.
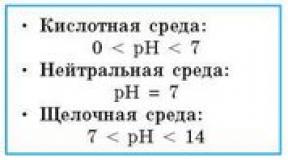
Depending on the method of contact with contaminated blood, there is a high, low and very low risk of disease. If the skin is pierced with a sharp object that has contaminated blood, or if a person is bitten by a sick person whose saliva contains blood, there is a high risk of infection. Getting blood into the eyes, mouth, nose, or onto a cut, abrasion, or scrape indicates a low risk of disease. Blood coming into contact with healthy, intact skin is considered to be a very low risk of infection.
Preventive measures aimed at reducing the possibility of infection with blood-borne diseases are: sanitary and educational education among the population, prevention, proper sterilization of medical instruments, prickly and cutting objects, widespread use of disposable syringes and needles, use of personal protective equipment by medical personnel in contact with infected people people, careful monitoring of donor blood.
In case of blood infections, pathogens circulate in a closed circle of the circulatory system and therefore do not have a free exit from the patient’s body.
Plague - a particularly dangerous infectious disease caused by the plague bacillus (bacterium from the genus J. pestis) is a vector-borne zoonotic disease. The stick dies when exposed to conventional disinfectants.
The incubation period of plague is 2-3 days, rarely up to 6 days. Forms of the disease: bubonic (inguinal lymph nodes are affected), pulmonary, intestinal. When a person is infected in natural foci, bubonic or septicemic plague develops, which can be complicated by secondary pneumonic plague. With airborne transmission of the pathogen from patients with secondary pneumonic plague, primary pneumonic plague develops.
The possibility of spreading the plague pathogen is associated with the following features:
A) short incubation period of the disease;
B) rapid development, often sudden development of a severe clinical picture of the disease and high mortality;
C) the difficulty of differential diagnosis in the first days of the disease;
D) the possibility of creating persistent foci of infection as a result of the presence of infected fleas and rodents in them.
For outbreaks of plague, the most dangerous form of plague is the pneumonic form of plague, but multiple simultaneous occurrences of the bubonic form of plague are possible. These epidemics begin with a previous epizootic (spread of plague) among rodents.
The entrance gates for plague are the skin, mucous membranes of the eyes, respiratory tract, and gastrointestinal tract. The disease begins acutely: chills, severe headache, heat, with the bubonic form - pain in the groin or under the armpit, with the pulmonary form - severe shortness of breath, chest pain, bloody sputum. Sleep is disturbed, aches in the muscles and joints, tachycardia and increasing shortness of breath appear. At the height of the disease, signs of toxic damage to the central nervous system and cardiovascular system come to the fore. The pulmonary form is the most dangerous for the patient and others, often ending in death. The intestinal form occurs when eating meat from sick animals.
Patients and persons in contact with it are subject to immediate isolation. A quarantine is established in the outbreak. Disinfection, disinsection, and deratization are widely carried out. Vaccinations are of great importance among the activities carried out. Contact people are given antibiotic therapy.
On the territory of Russia there are the following natural foci of plague: 1) Northwestern Caspian region (the main source is the ground squirrel); 2) Volga-Ural (gerbil); 3) Trans-Ural (gerbil); 4) Transcaucasian (gerbil); 5) Gorno-Altai (gophers and marmots); 5) Transbaikal (tarbagany); 6) Tuvan.
Typhus. The causative agent is rickettsia. The source of infection is a sick person, the transmitter is a body louse. The incubation period is 7-20 days. Symptoms - chills, headache, loss of consciousness, delirium, from the 5th day - a rash on the sides of the body.
The patient must be hospitalized. The outbreak is disinfected and disinfested, people who have been in contact with the sick are sanitized, and they are monitored. Vaccinations are being carried out.
Malaria. The causative agent is Plasmodium malaria, the carrier is a mosquito. It is not directly transmitted from patient to patient, but only through a mosquito. The incubation period is 1-3 weeks, sometimes 7-12 months.
Symptoms are sudden attacks of chills, fever, sweating, pain in the joints, muscles, and in the spleen area. The attacks last 6-10 hours and occur again with a certain frequency, depending on the form - three-day, four-day, tropical. The patient must be hospitalized. To prevent the disease - identifying and treating patients, as well as mosquito control. All those who were ill in the past year are given anti-relapse treatment in the spring, and then chemoprophylaxis throughout the entire period of mosquito activity.
Tick-borne encephalitis. The causative agent is a filter virus. The reservoir and carriers are ticks, as well as chipmunks, mice, moles, hedgehogs, and some birds. The virus is transmitted through tick bites. The incubation period is 10-14 days. The disease is seasonal - in spring, summer - due to the activity of ticks during this period.
Symptoms - severe headache, high temperature - 39-40 0, nausea, vomiting, convulsions, unconsciousness. There may be paralysis of the limbs. Mortality rate – 25%. After recovery, strong immunity remains. Prevention – vaccinations, protection against ticks, use of anti-tick products. When working in the forest, inspections and mutual inspections are required every 1.5-2 hours.
AIDS– an infectious viral disease transmitted through blood (transfusion of infected blood, injections, in dental offices, most often through sexual intercourse). There are patients who die quite quickly, and infected people who are carriers of the virus. The disease causes the body to lose its immunity and protective properties, and therefore indolent infections develop - sore throat, pneumonia, sudden weight loss, and in some patients sarcoma develops. There are no specific means of treatment and prevention yet. Risk groups are being checked for treatment of HIV infection, preventing the possibility of infection, checking donors, disposable syringes, etc.
Traditionally, human immunodeficiency virus (HIV) has been the main focus of pathogens transmitted through contact with contaminated blood, but the rise in the incidence of hepatitis C in North America has meant that hepatitis is now the most common disease transmitted by this route.
Currently, infection with the hepatitis B virus, which has been considered an occupational pathology for surgeons for almost 50 years, less often leads to the development of the disease, which is associated with the spread of vaccinations and the development of a relatively effective treatment regimen in case of contact with the virus.
2. What is the comparative risk of contracting HIV, HBV and HCV?
A) HIV. Currently, approximately 1 million people in the United States are infected with HIV. Recent observations indicate that transmission of HIV in hospital settings is rare. Health care workers make up only 5% of all AIDS patients, and most of them have factors other than occupational ones that likely caused the disease. The greatest occupational risk was observed among nurses and laboratory workers.
Since January 1, 1998, there has not been a single documented case of HIV transmission from patient to doctor as a result of professional contact.
b) HBV. There is no doubt that all surgeons are exposed to HBV during their normal working career. It is believed that 1.25 million people in the United States have chronic hepatitis B. Percutaneous injection with a contaminated needle leads to acute disease in approximately 30% of cases. In 75% of cases, hepatitis B is clinically hidden, and 10% of those infected remain carriers of the virus for life.
Many carriers, who are potentially infectious to others, are asymptomatic with minimal or no progression. In approximately 40%, the disease continually progresses, leading to cirrhosis, liver failure, or even genocellular carcinoma.
V) HCV. Hepatitis C has become the most main problem. Chronic hepatitis C is believed to affect approximately 4 million people in the United States. The risk of seroconversion from percutaneous injection with an infected needle is about 10%, but in 50% acute disease leads to chronic carriage of the infection. The course of hepatitis C still exists different opinions However, in almost 40% of patients, chronic HCV infection leads to the development of cirrhosis.
In the latter case, there is a high risk of developing liver cancer, the probability of which reaches 50% within 15 years.
3. Does hepatitis B vaccination provide complete protection against the disease?
Effective hepatitis B vaccination is now available to all surgeons and operating room staff. Hepatitis B vaccine is produced using recombinant technology; it is not destroyed virus particles obtained from infected people. Three doses of the vaccine are administered, after which the titer of surface antibodies should be determined to ensure the success of vaccination.
Approximately 5% of vaccinated people do not develop antibodies and require a booster vaccination. Some people remain refractory to vaccination and remain at risk of acute hepatitis B. Vaccination does not guarantee immunization.
According to some studies, 50% of practicing surgeons do not have sufficient immunity to HBV due to various reasons: lack of vaccination in older surgeons, more than 5 years after vaccination, insufficient amount of recombinant vaccine or improper vaccination and, finally, inability to develop the appropriate immune answer.
4. Is there a risk of infection of patients from surgeons infected with HBV?
Transmission of hepatitis B virus from surgeon to patient has been documented. The blood test of surgeons who can infect patients is usually positive for the e-antigen of the hepatitis B virus. The E-antigen is a breakdown product of the viral nucleocapsid and indicates active replication of the virus in the liver. Detection of the e-antigen indicates high titers of the virus and the relatively high infectiousness of the patient.
The large number of documented cases of transmission of hepatitis B to patients from persons involved in surgery may cause particular problems and limitations in clinical activities for clinicians who transmitted this infection. One of the latest reports from England reports the transmission of hepatitis B virus to a patient even from a surgeon with a negative HBV e-antigen test.
IN Lately One national organization is calling for restrictions on the activities of E-antigen-positive surgeons. The question of whether a surgeon with chronic hepatitis B can continue to practice will be discussed in the future.
5. What is the correct tactic for percutaneous contact with the blood of a patient who has hepatitis B?
Tactics depend on the health worker’s vaccination status. If he is vaccinated and has a positive antibody titer, then nothing needs to be done. If the health care worker is not vaccinated and does not have antibodies to HBV, he or she should be given a dose of anti-HBV immunoglobulin and begin the hepatitis B vaccination series.
Health care workers who have previously been successfully vaccinated against hepatitis B but have no or negligible antibody titres should receive a dose of anti-HBV immunoglobulin and a repeat dose of hepatitis B vaccine. Since in most cases of such contact the patient is not known whether he is infected or not, then, in general, surgeons need to know whether they have antibodies and periodically repeat immunization against hepatitis B every 7 years.
6. How is HCV different from HBV? Which one is more dangerous?
A) Incidence in the USA:
- HBV: approximately 1.25 million patients.
- HCV: approximately 4 million patients.
b) Path and consequences of infection:
- HBV: DNA blood-borne virus; the acute form becomes chronic in 10% of cases.
- HCV: blood-borne RNA virus; the acute form becomes chronic in 50% of cases.
V) Prevention:
- HBV: effective recombinant vaccine.
- HCV: There is currently no vaccine.
G) Protection after contact:
- HBV: for people who have not been vaccinated and do not have antibodies to HBV, it is advisable to receive anti-HBV immunoglobulin.
- HCV: the clinical effectiveness of anti-HCV immunoglobulin has not been proven. Among the patients treated by surgeons in the United States, more people have chronic hepatitis C than chronic hepatitis B, and there is no vaccine against HCV infection. The risk of seroconversion for hepatitis C is 10% versus 30% for hepatitis B, but HCV infection is much more likely to become chronic (50% versus 10%). Therefore, HCV infection poses a much greater threat to surgeons.
7. How high is the risk for a healthcare worker to become infected with HIV?
The first case of HIV infection of a health care worker was recorded in 1984. By December 1997, epidemiological centers had received approximately 200 reports of occupational exposure. A study of these cases found that 132 health care workers had non-occupational risk factors, and only 54 had documented transmission.
Transmission of infection was confirmed if a healthcare worker had contact with the blood or body fluids of an infected patient, after which HIV seroconversion was noted. The occupational risk is certainly higher for nurses and laboratory workers. The total number of infections does not compare with the large number of exposures to the virus that appear to have occurred since the beginning of the epidemic (early 1980s).
8. Is there less risk of HIV infection when performing laparoscopic operations?
Recently, laparoscopic surgery in HIV-infected patients is considered a good replacement for open interventions. This method reduces the likelihood of contact with blood and sharp instruments, however, due to some of its features, it is possible for surgeons to become infected in other ways than during a conventional operation. When desufflating pneumoneritoneum during laparoscopic interventions, droplets of HIV-infected blood are splashed into the operating room. The risk of contamination can be reduced by directing air into a closed system and taking appropriate precautions when changing tools.
9. Is double gloving an effective method of protection?
Due to the possibility of broken skin coming into contact with blood, the risk of infection of people working in the operating room with the hepatitis virus or HIV is increased. While double gloving may not prevent skin damage, it has been shown to clearly reduce the likelihood of blood exposure. Studies of exposure to blood in the operating room have shown that 90% of exposure occurs on the skin of the surgeon's hands distal to the elbow, including the area protected by gloves. According to one study, if a surgeon wears two pairs of gloves, the likelihood of his skin coming into contact with blood decreases by 70%. A puncture of the outer pair of gloves was observed in 25% of cases, while a puncture of the inner pair was observed only in 10% (8.7% for surgeons and 3.7% for assistants). Puncture of the inner pair of gloves was observed during operations lasting more than 3 hours; it was always accompanied by a puncture of the outer pair. The greatest damage occurred on the index finger of the non-dominant hand.

10. Is droplets getting into the eyes a big threat to surgeons?
A study of epidemiological centers showed that approximately 13% of documented transmission cases involved contact with mucous membranes and skin. Droplet contact with the eye is often underestimated, although this type of contact is the easiest to prevent. A recent study looked at 160 pairs of eye shields used by surgeons and assistants. All operations lasted 30 minutes or more. The number of droplets was counted on the screens, first macroscopic, then microscopic. Blood was found on 44% of screens tested. Surgeons noticed spatter in only 8% of cases. Only 16% of the droplets were visible macroscopically. The risk of droplets entering the eyes was higher for the surgeon than for the assistant and increased with increasing operative time. It has been proven that the type of intervention is also important: the risk is higher in vascular and orthopedic operations. Eye protection should be mandatory for everyone working in the operating room, especially for those directly operating.
11. How often does the surgeon’s blood come into contact with the patient’s blood and body fluids?
Contact with blood is possible in case of damage to the skin (injections, cuts) and contact with the skin and mucous membranes (puncture of gloves, scratches on the skin, droplets getting into the eyes). Contact due to skin damage is observed in 1.2-5.6% of surgical procedures, and contact due to contact with skin and mucous membranes - in 6.4-50.4%. The differences in the numbers reported are due to differences in data collection, procedures performed, surgical technique, and precautions. For example, surgeons at San Francisco General Hospital take extreme precautions, wearing waterproof uniforms and two pairs of gloves. There have been no cases of transmission of infection to any health care worker through contact of his intact skin with infected blood and biological fluids. However, healthcare workers without other risk factors have been reported to become infected with HIV due to contact with their mucous membranes and skin of HIV-infected blood. The likelihood of transmission of infection through such contact remains unknown, since seroconversion was not observed in health care workers after contact of their mucous membranes and skin with HIV-infected blood in prospective studies.
The risk of infection exists for everyone working in the operating room, but it is much higher for surgeons and first assistants, since they account for 80% of skin contamination and 65% of injuries.
12. Is skin contamination explained only by surgical technique?
Scratched skin may come into contact with blood or body fluids even when all precautions are taken. Unfortunately, not all protective clothing provides equal protection. One study noted defects in 2% of sterile surgical gloves immediately after unpacking them.
13. What is the probability of seroconversion after exposure of a healthcare worker's blood to a patient's blood for HIV and HBV?
The chance of seroconversion after a needle stick is 0.3% for HIV and 30% for HBV.
14. What is the likelihood for a surgeon to become infected with HIV on the job during his career?
The risk of HIV transmission to a surgeon can be calculated by knowing the rate of HIV detection in surgical patients (0.32-50%), the probability of skin damage (1.2-6%) and the probability of seroconversion (0.29-0.50%). Thus, the risk of contracting HIV from a particular patient ranges from 0.11 per million to 66 per million. If a surgeon performs 350 surgeries per year for 30 years, his lifetime risk of infection ranges from 0.12% to 50.0%, depending on variables. There are several assumptions made in this calculation.
Every person wants to live their life brightly and interestingly. But many don’t even want to think about the consequences. A stormy and active sex life can often “give” a lot of unpleasant surprises.
Currently, scientists know more than 20 types of STDs of various types. If we remember the distant 70s, our parents had information about only two diseases that were transmitted “through the bed.”
Viruses can be divided into:
- Incurable
- Curable
Scientists around the world are trying to create drugs and antibiotics to cure these diseases, but many remain “killer”. Almost half of the people who contracted the disease through sexual intercourse were under 30 years of age.
The seven most dangerous sexually transmitted diseases
Immunodeficiency of the body, the last, fatal stage of this disease is called AIDS. Viruses in the body can develop in a latent form, more slowly or rapidly. The body exhibits tumors and multifocal infections caused by protozoan bacteria and fungi. They may not affect a healthy person, but they are deadly for someone infected with HIV.

A healthy person has a strong immune system; a sick body has a weakened immune system that is unable to fight infection. AIDS cannot be cured. It is possible to support the immune system with special drugs and medications, but the cost of such treatment is very high. Routes of transmission: through unprotected sexual intercourse, through blood and syringes, in some cases from mother to child.
An STD that is caused by the microorganism Triponema pallidum. A person with syphilis does not even know about his illness for the first month. The incubation period of the virus is about 30-35 days. The disease manifests itself on the skin in the form of eczema, spots, and purulent wounds. Further, it affects internal organs, mucous membranes, nervous system and bones.

Chlamydia
Today it is the most common disease. The causative agent of the infection is the intracellular organism chlamydia. You can become infected with this disease in several ways: unprotected sexual intercourse (instantly), through a towel and bed linen of the patient (using secretions), during childbirth from mother to baby.
A sign of chlamydia: abundant unpleasant purulent discharge from the genital tract, sharp pain in the lower abdomen, pain and pain in the vagina may be accompanied by short-term and heavy bleeding. Many of the patients who have had chlamydia remain infertile.

This disease can provoke and develop the following diseases: the appearance of atherosclerosis, bone destruction, pain in the spine, of varying complexity vascular diseases, diabetes, deterioration and loss of vision.
The causative agent of the disease is a dangerous microorganism, gonococcus. Signs of the disease in men appear on the 4th day after infection. This disease can be recognized by a sharp pain during urination. The external opening is covered with a dense film of mucus and pus. In women: on the 5th day you can see unpleasant mucus with pus in the vagina.

Heaviness appears and It's a dull pain in the lower back, lower abdomen. Many women may experience intermenstrual, light discharge and bleeding. If left untreated and not examined, gonorrhea can lead to inflammation of the uterus, appendages, and infertility.
Grip can be transmitted not only through sexual contact, but also through personal items (bed linen, dishes, cutlery, towels, underwear, toothbrush, washcloth).
Doctors call this disease “type 2 herpes.” This serious viral disease affects the entire body. The inflammatory process begins on the lips, then spreads to all other mucous membranes. Very often, with this disease, immunity decreases. The disease instantly spreads to the genitals, eyes, intestines, liver and even the brain. This virus does not develop rapidly and cannot be removed from the body. Routes of transmission: during sexual intercourse, through contact with affected areas of the skin of the hands and lips.

Ureaplasmosis
The carriers are ureaplasma. Symptoms of the disease are subtle, develop slowly, and are hidden. Many carriers of this virus may not take their illness seriously. Under stress and decreased immunity, the virus begins to “work” faster. Ureaplasma can disrupt sperm activity.

This disease is very dangerous for pregnant women. Many doctors suggest getting rid of the fetus. The incubation period of the virus is from one to two months. Signs of a urinary infection: a slight burning sensation when urinating, white or clear discharge, inflammation of the genital organs, pain during sex.
A dangerous disease for all humanity. Every year, 3 million people worldwide fall ill with this virus. This virus is the most resistant to the external environment. The virus persists on a dried blood stain, on a razor blade, or on a needle for up to 10 days.
At the first stage of development of the virus, it can be compared to the mild stage of acute respiratory infections. After a couple of days, the infected person loses appetite, lack of strength, lethargy, joint pain, headache, urine becomes dark in color, signs of nausea and vomiting appear.

The chronic course of the disease is characterized by: pain in the right hypochondrium, enlarged liver, skin itching, change in body cover to a more unnatural color (yellow). In the chronic form of Hepatitis B, it is necessary to strictly follow all doctor’s instructions, follow a special diet, and give up tobacco and alcohol.
Unprotected sexual intercourse – 80% that infection will occur instantly. Random unprotected (oral, anal) relationships entail dire consequences. Prevention of this kind of disease can only be done through careful and protected sexual intercourse. Washing the genitals with water and interrupting sexual intercourse cannot be protection against STDs. The absence of symptoms of illness does not mean your partner is completely healthy. Trust but verify your partner.
Read also...
- M. V. Koltunova language and business communication. Language and business communication Etiquette and protocol of business communication
- The Last of the Mohicans Fenimore Cooper The Last of the Mohicans
- Descriptive phrase for the word flower
- Mikhail Zoshchenko - Don't lie: Fairy tale Don't lie Zoshchenko genre